Summary
A routine surgery leads to a puzzling reaction. Is more surgery required, or is it something else?
Guests

Steven Chen, MD, MPH
Steven T. Chen is a board-certified internist and dermatologist at Massachusetts General Hospital. He is Assistant Professor of Dermatology at Harvard Medical School.
Dr. Chen graduated with Honors from Johns Hopkins University where he earned a bachelor’s of science in Biology. He subsequently earned a Masters in Public Health (MPH) and a medical degree (MD) at Johns Hopkins, and was elected to the Alpha Omega Alpha Honor Society. He then pursued residency training at Harvard, where he completed an Internal Medicine residency at Beth Israel Deaconess Medical Center and a Dermatology residency in the Harvard Combined Dermatology Program. He served as Administrative Chief Resident during his final year of combined training.
He belongs to several professional organizations, including the American Academy of Dermatology, the United States Cutaneous Lymphoma Consortium, and the International Society for Cutaneous Lymphomas. He pursues clinical and education research and has co-authored peer-reviewed articles in medical education and complex dermatology. His clinical interests include cutaneous lymphomas, complex medical dermatology, inpatient dermatology, and medical education.
Dr. Chen attends on both the dermatology and internal medicine services. He is the Co-director of the Comprehensive Cutaneous Lymphoma Program, and serves as Director of Medical Education and Director of the Blistering Orders Clinic in the Department of Dermatology.
Transcript
DDx SEASON 2, EPISODE 7 TRANSCRIPT
When an infection isn’t an infection
[Intro music]
Raj: A 64-year-old woman has routine gallbladder surgery. While recovering, she becomes febrile and develops a rash at the surgical site.
[Music]
Raj: This is DDx, a podcast from Figure 1 about how doctors think. This season is all about dermatology. I’m Dr. Raj Bhardwaj. Today’s case comes from Dr. Steven Chen, who we heard from earlier this season.
Steven Chen: I am a board certified dermatologist and internist. I work at Massachusetts General Hospital, here in Boston, Mass., and Harvard Medical School.
[music]
Raj: The patient had been seen at a nearby facility for a run-of-the-mill operation.
Steven Chen: and had undergone a pretty standard surgery. She had gotten a laparoscopic cholecystectomy. During that process afterwards, she ended up developing fevers and ended up developing a rash on her abdomen
Raj: But even routine surgery carries with it the risk of complications.
Steven Chen: I don’t know the exact circumstances of the surgery, but what I do know is that she ended up having to go back to the operating room to have an open cholecystectomy, and then had a drain placed in the right upper quadrant. And then this rash kept progressing. So all we knew at the time when we were paged about this patient was that there was someone coming from another hospital with fevers, with a rash on their belly and a concern that there was a spreading infection.
Raj: When Dr. Chen arrived, he conducted a thorough physical exam and immediately found a clue.
Steven Chen: She had her drain in place. And this rash was basically at every single port site. So everywhere that she had an incision, she had an expanding rash.
Raj: He noticed a clear correlation between the incision sites and the affected tissue.
Steven Chen: She had these large ulcerations that had an erythematous, violaceous, or gunmetal gray border. And aside from that just, lots and lots of inflammation and lots of purulent drainage, especially coming from the open cholecystectomy site. Nothing had been closed. So everything was still open at this point. And so what we were dealing with was a large wound on the abdomen at the open cholecystectomy site. This expanding, painful, violaceous, ulcerative rash, and obviously this drain that was in place.
Raj: The rash was aggressive. It had already spread to a large part of the patient’s trunk.
Steven Chen: You can imagine that these large ulcers covered so much of her abdomen. The largest one was probably at least 20 centimeters in diameter because of the fact that the scar was open at that point. And then every other site where she had a port, she had another large ulcer of at least 10 centimeters. So if you just looked at her belly, a good probably 60 to 75 percent of it was replaced by this ulcer.
Raj: The team needed to act fast. But what exactly were they dealing with?
Steven Chen: I think the decision to treat really depends on your specialty. If you’re a dermatologist or if you’re an internist and you think it’s an infection, one of the first things you might think about is giving antibiotics. If you’re a surgeon and you see that, one of the first things you might think about is actually debridement — taking them back to the operating room to take out more tissue.
[Music]
Raj: The admitting staff thought they recognized this, and knew to page dermatology instead of infectious disease.
Steven Chen: She was admitted to the surgery service, and to their credit, they took one look at her and called dermatology right away because I think they suspected the same thing that we ended up diagnosing her with. And that was a critical move. And I’ll explain why. So when we first saw her, she was in immense pain, 10 out of 10 pain. It was really difficult to fully examine her because of all that pain. And she had literally just hit the floor and the primary surgery team who had just paged us was in the room with us taking a look at her.
Raj: This looked a lot like something they had seen before.
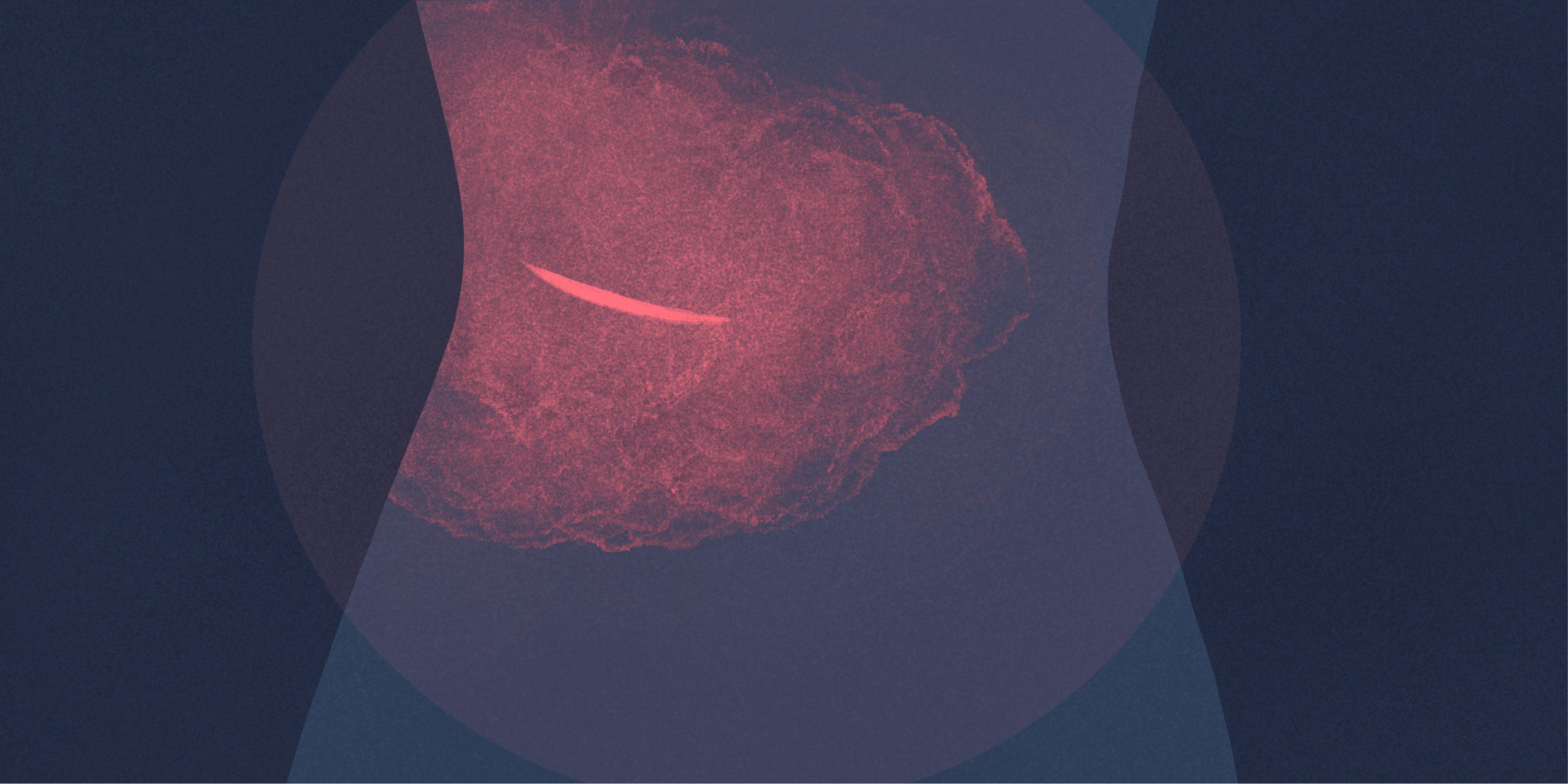
Steven Chen: The primary team had consulted us out of a concern for pyoderma gangrenosum. And upon seeing her, our first thought was that, yeah, this looks pretty good for PG, for pyoderma gangrenosum, but it’s hard to rule out an infection, especially when someone has fevers and this much pain and this type of what really looks like a necrotic eruption, basically looks like the skin was dying.
Raj: Pyoderma gangrenosum is a rare condition associated with inhibited immune system function, and characterized by a rapidly growing ulcer.
Steven Chen: So as is customary for us on the consult service, we ended up trying to do a full skin exam so that we could take a look everywhere else. And the thing that really helped us was on her left shin. So on her left shin, she had a separate skin finding that was also ulcerative, but there was much less inflammation. And most importantly, there was scarring that appeared in a cribriform manner, meaning that it really looked almost like a net, like this scar was occurring in these bridges of skin that were coming into the ulcer. So after seeing that, it really helped us confirm her diagnosis. This really all looked like pyoderma gangrenosum. And this is another one of those cases where a misdiagnosis can be truly detrimental. And in some rare cases, fatal.
[Music]
So we know that pyoderma gangrenosum is a neutrophilic dermatosis, which just means that a ton of neutrophils end up flooding into the skin and it can cause these ulcers. They usually start as a little pustule or like a pimple and then they spread from there. But the classic exam finding, which we saw with this patient, is that violaceous, that really purplish look. And then just the expanding nature of it and the pain and the ability for it to come with fevers really helped us with our diagnosis in this case.
Raj: Pyoderma gangrenosum typically develops in middle-aged people, and is prone to recurring.
Steven Chen: Sometimes people just have bad luck and they get a terrible diagnosis like this. And sometimes it’s really something driving it underneath. And when there is an underlying driver or a trigger, the most important thing is to remove that trigger either by treating it or to take it away. Be it like a drug or an antigen.
We know that in this instance she had because she had something on her leg. What that told me is that she did have p.g in the past, but maybe it was never diagnosed.
Raj: PG often starts with small red bumps or blisters on the skin, which erode into painful ulcers. And it’s often associated with some other condition…
Steven Chen: So the most common thing that we think about as a trigger for pyoderma gangrenosum is inflammatory bowel disease or more specifically, ulcerative colitis and of course, Crohn’s disease as well. But that’s what we all learn in medical school. And after graduating and after practicing for a few years, you start to realize that not everyone has a clear trigger that’s identifiable. And so it’s our job to try to figure out what that trigger might be, but also to know when we’ve kind of turned over enough rocks, when we’ve done enough of a workup and to focus on the therapy, to make the patient feel better and to make their skin heal, all the while knowing that we still have to have that in the back of our minds, knowing that we’re not missing something that could be fueling everything.
And so the surgery is really what tipped her over the edge in terms of developing all of these new spots on her belly.
Raj: Confirming the diagnosis of pyoderma gangrenosum can be difficult, because it looks like an infection, even under a microscope.
Steven Chen: And this is why it’s so confusing. It’s because if you send the specimen to pathology, there’s really no way for them to say that it looks perfect for pyoderma gangrenosum because it’s a ton of neutrophils. So it really looks like an infection under the microscope as well. And so for that reason, we always hear horror stories of surgeons who continually take their patients back for debridement over and over again, not realizing that what they’re dealing with is actually an autoinflammatory neutrophilic dermatosis called PG, as opposed to an infection. And these patients end up in this vicious cycle where every time they go back, more gets taken. It gets read out as a possible infection. And then here’s the worst part of it, is that if you do anything to traumatize that ulcer, if you do anything to disturb a neutrophilic dermatosis, it actually gets worse, which is what we call pathergy. And so it just ends up you end up setting up this vicious, never ending cycle when these patients end up going to the O.R. over and over again.
[Music]
Raj: Fortunately, Dr. Chen and the surgical staff had enough experience with PG to take appropriate action.
Steven Chen: in this case, luckily, like I mentioned, our surgeons were quite astute, noticed it and thought PG and immediately called us. And together in the room, we devised a plan which was to start high-dose systemic steroids for her to try to shut down this inflammation so that she could start healing. And so we started systemic steroids in an I.V. form, kept her in the hospital to make sure she was turning the corner, watched as her fever went away, as the inflammation, that redness, that violaceous color started to fade.
Raj: Even with the proper treatment, the patient’s path to recovery was protracted. Remember, these ulcers covered almost 75 percent of her abdomen.
Steven Chen: The problem, as all dermatologists know is that these large, large ulcers take a long time to heal, and so she ended up getting discharged to a rehab and then going home. But all the while with nursing care to help her with the very chronic nature of these wounds. I followed her in the outpatient setting and it really took her a full year before everything was completely healed up. But now she’s able to look back on this experience and know what exactly she was dealing with.
[Music]
Raj: So how can you recognize PG if you’ve never seen it before?
Steven Chen: The classic exam for pyoderma gangrenosum, it kind of depends on if it’s really early or if it’s already had some time to evolve. But if it’s very early. Just again, it looks like a pimple. It just looks like a little bump with some pus in it. Just because we know that it’s a neutrophilic dermatosis, so all those neutrophils are just creating that purulence, and it basically is surrounded by this very deep purple inflammation. The classic appearance of PG that we think about when we think about it in a more ulcerated form is obviously an ulcer, but the border is very actively inflamed with deep purple, violaceous, and the classic words that we use are gunmetal gray appearance. So it just looks so purple that it almost looks grayish at that point. And then the border has a rolled border. So what that means is that if you’re looking at the ulcer, for example, on cross section, like from the side, you could actually see the border hanging over the ulcer a little bit. The way I describe it to our medical students and our residents, it’s as if you could take a little Q-Tip and poke underneath it. And there is… you’re basically able to poke a little bit and get between the border and the actual base of the ulcer.
Raj: If something is behaving strangely, take a step back and consider what else is on your DDx. As the old saying goes, when you hear hoof beats, think horses, not zebras. But keep in mind that zebras do exist.
Steven Chen: For people who are not familiar, for the healthcare professionals who are not familiar with this diagnosis, it’s the recognition that this exists. And it’s to know that when you have, especially for those of us who might operate, who might perform surgery. But for those of us who in that case might be thinking about a postoperative infection, is to always think about this on your differential diagnosis, too. I’m not saying that you shouldn’t treat for infection and you shouldn’t debride the wounds, but I think if things aren’t acting the way that they should, it’s a good time to think about pyoderma gangrenosum, and I’d also put a plug in as a good time to call a dermatology consultant to help you, because it’s possible that you may be dealing with one of these auto inflammatory disorders instead.
CREDITS
Thanks to Dr. Steven Chen for speaking with us.
This is DDx, a podcast by Figure 1.
Figure 1 is an app that lets doctors share clinical images and knowledge about difficult-to-diagnose cases.
I’m Doctor Raj Bhardwaj, host and story editor of DDx. You can follow me on Twitter at RajBhardwajMD
Ddx is produced by David Crosbie for Earshot Podcasts.
Sound design and mixing by Chandra Bulucon.
Our theme music is by Nathan Burley.
The executive producers of DDx are Jesse Brown and Kevin Sexton.
Head to Figure1.com/ddx, where you can find full show notes, photos, and speaker bios.
Thanks for listening.