DERMATOLOGY
Psoriasis Comorbidities
Clinical Guidelines and Resources
Sign up for Figure 1 and be notified directly of new clinical cases and related research, CME activities, quizzes, news, and trends. It’s free!
Figure 1, 2, 3

1. All patients should be screened for psoriatic arthritis at each visit

2. Psoriasis can cause significant psychosocial stress on a patient

3. Patients are about twice as likely to have irritable bowel syndrome or ulcerative colitis than people without psoriasis
Summary
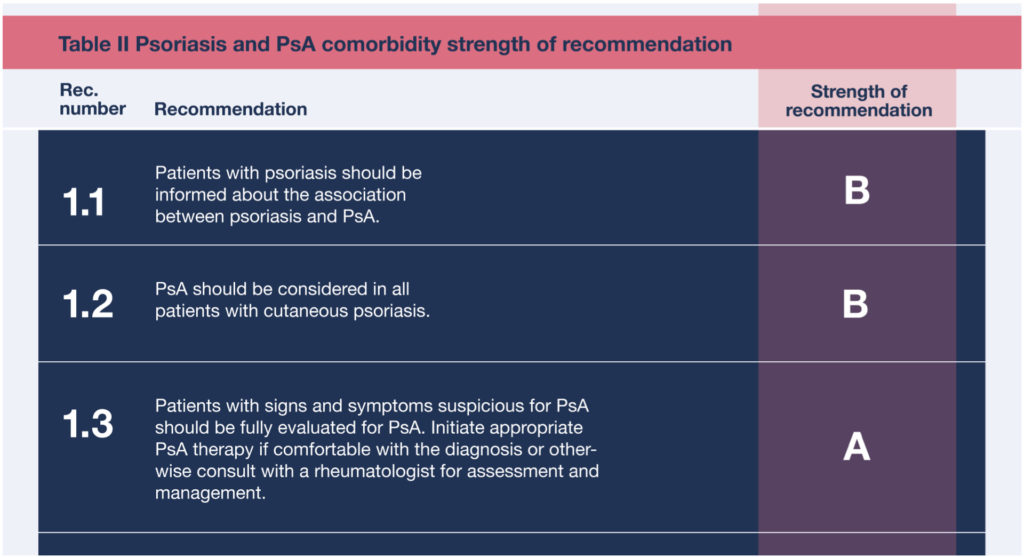
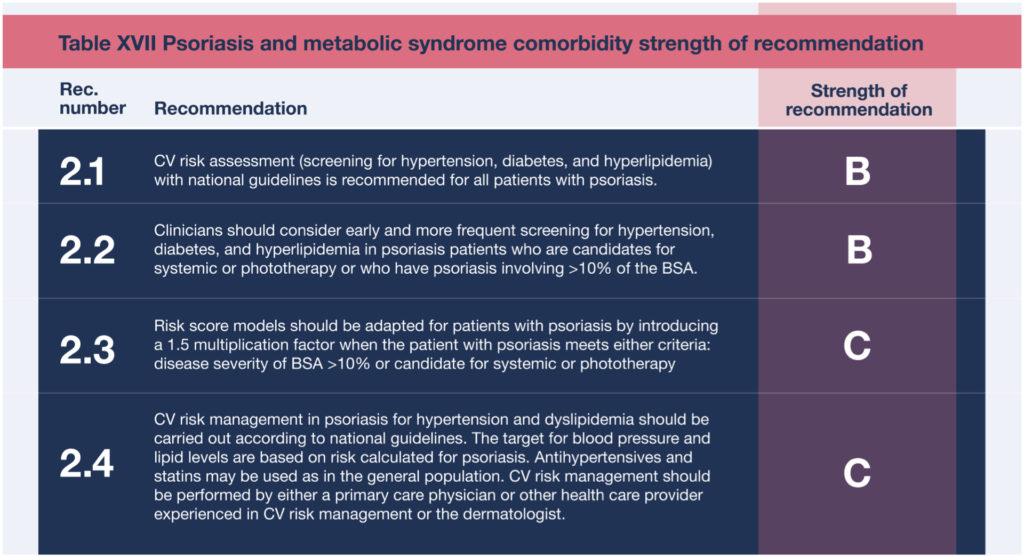
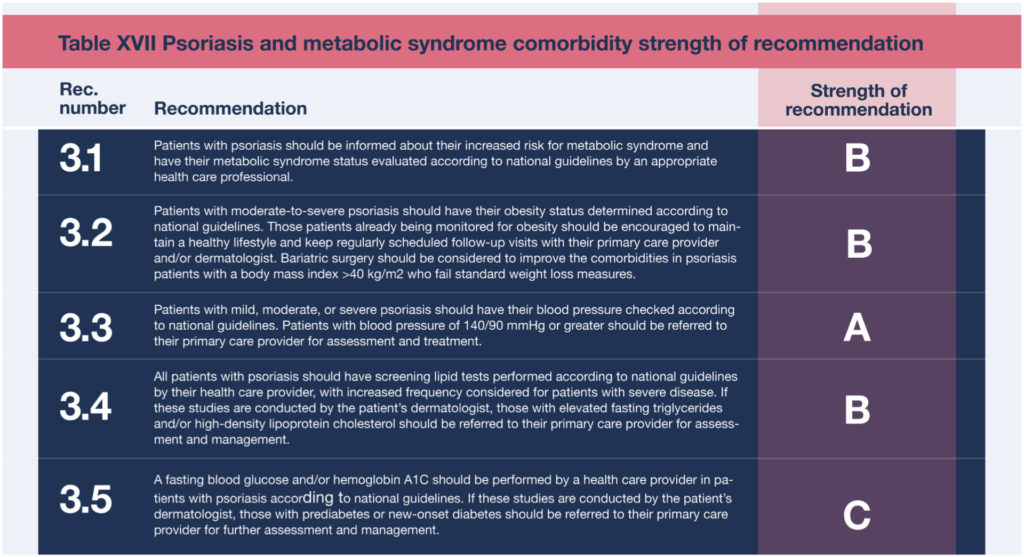
After more than a decade, the American Academy of Dermatology (AAD) and the National Psoriasis Foundation (NPF) updated their guidelines for managing and treating psoriasis, including psoriasis comorbidities. Here’s a brief summary of some key recommendations coming out of the revised guidelines related to psoriasis and comorbidities.
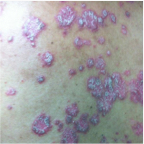
First, all patients with psoriasis should be screened for psoriatic arthritis at each visit. Both dermatologists and patients should be familiar with psoriatic arthritis symptoms, such as unexplained morning joint stiffness or swelling. Joints in the hands, feet, knees, wrists, and elbows, as well as the spine can all be affected, and the symptoms may resemble other conditions such as rheumatoid arthritis and ankylosing spondylitis. The key is to catch psoriatic arthritis symptoms early. Cutaneous symptoms can arise years before any arthritic symptoms arise, but if arthritic symptoms present and go untreated, they can cause irreversible joint damage.
Psoriasis Comorbidities Clinical Guidelines and Resources
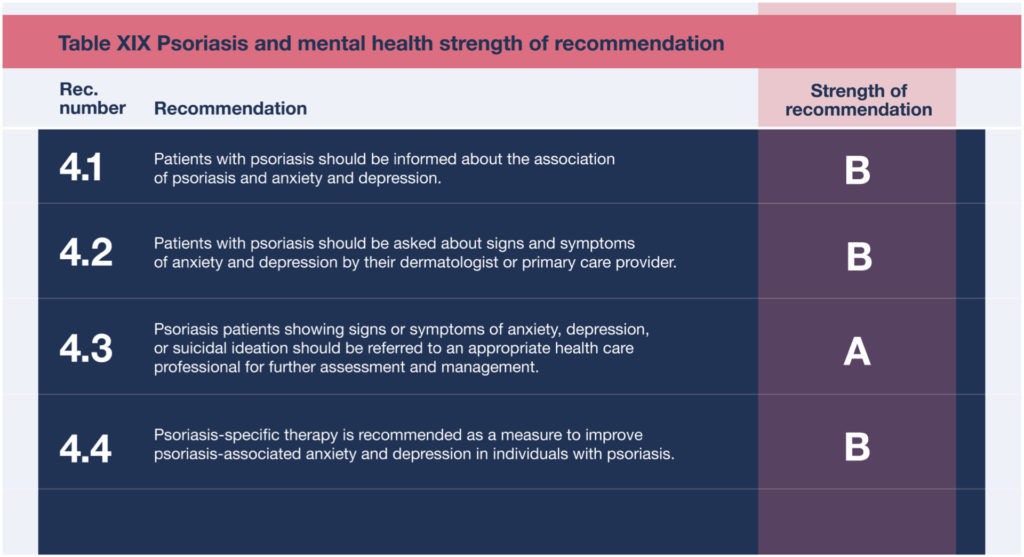
Psoriasis can also cause significant psychosocial stress on a patient, and it may affect their personal relationships, sexual activity, and professional performance. Patients are 50% more likely to develop depression than people without psoriasis. Dermatologists should be aware of how a patient’s condition is affecting their quality of life, and should look for signs of anxiety and depression. Patients may be unwilling to initiate a conversation regarding their mental health out of fear their concerns may be dismissed or stigmatized. Dermatologists should take the first step and ask patients how their condition has impacted their mental health, and validate their patient’s concerns and experiences.
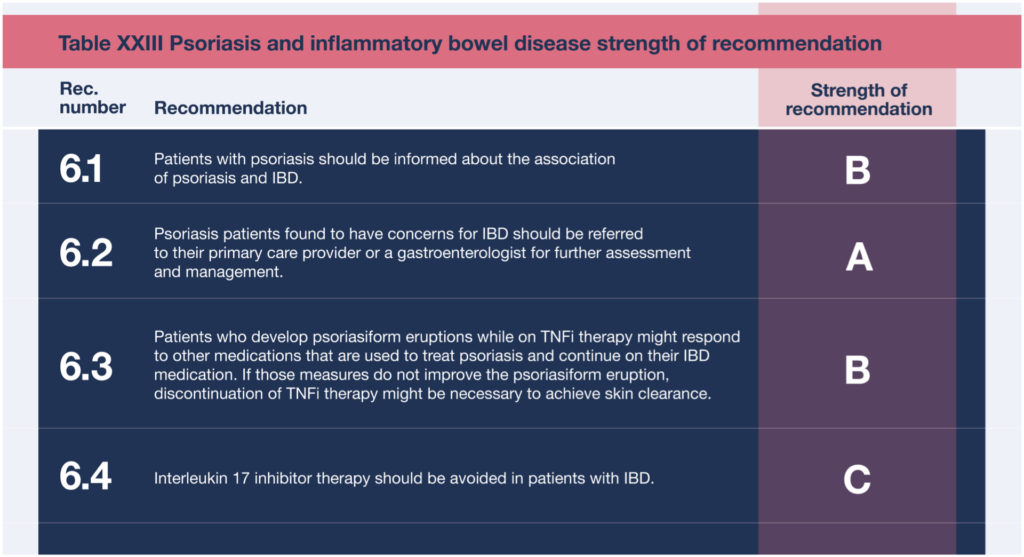
Those with this condition are about twice as likely to have irritable bowel syndrome or ulcerative colitis than people without psoriasis. Dermatologists should be aware of, and educate patients on the signs and symptoms of these diseases. Irritable bowel syndrome symptoms include abdominal cramps, bloating, diarrhea, and constipation that can not be explained by other conditions. Ulcerative colitis symptoms are similar, but may also include blood in the stool. If a patient reports symptoms like this, encourage them to consult their primary healthcare provider.
Psoriasis patients taking TNFi for irritable bowel syndrome are also at risk of developing psoriasiform eruptions. If these present, dermatologists should treat the patient on a case by case basis.
And patients are at risk for chronic renal disease. Patients should routinely get bloodwork done in order to monitor for kidney disease, such as elevated blood urea nitrogen, creatinine, and urine microalbumin. If these lab results do come back elevated, the patient’s primary care physician should be notified immediately.
Full Guidelines
Read the full guidelines on psoriasis comorbidities from AAD and NPF: Guidelines of Care for the Management and Treatment of Psoriasis with Awareness and Attention to Comorbidities
Strength of Recommendations

Psoriasis Comorbidity Patient Cases
Click on the image to see the full case details and sign in to view community comments.
See more cases like these
Sign up for Figure 1 and gain access to a library of 100,000+ real-world cases.

Psoriasis Clinical Quiz
Take this quiz in the app to test your knowledge and view community comments.
ww Quick Quizw
What proportion of patients with psoriasis may develop accompanying arthritis?
A 70-year-old female with psoriasis presents with a four-month history of worsening arthralgia. She mentions she has pain and stiffness in her big toes and most of her fingers. On examination, a telescoping finger deformity is seen on her right second digit. What proportion of patients with psoriasis may develop accompanying arthritis?

Learn by Listening
Psoriasis and Mental Health DDx Podcast Episode
Hear how psoriasis impacts much more than a person’s skin, and how misinformation only exacerbates the stigma.

Free CME
A Paradoxical Phenomenon CME Activity
Improve your early recognition and appropriate management of TNF-inhibitor induced psoriasis and increase your patient education and clinician awareness of risk factors, as well as the pathogenesis that may contribute to this paradoxical reaction. Start activity >
Free Dermatology CME
Sign up for Figure 1 and gain access to our continuously growing CME & Education Center full of visually interesting and unique CME activities.

Related Research
Beyond Skin Deep: Addressing Comorbidities in Psoriasis | PubMed
“Psoriasis is a chronic inflammatory disease that is commonly encountered in primary care and is associated with significant morbidity that extends beyond the skin manifestations … Enhanced recognition of these comorbidities may lead to earlier diagnosis and potentially better overall health outcomes … Effective therapies are now available that have been shown to concurrently improve skin disease, quality of life and psychiatric symptoms.”
Psoriasis: Comorbidities | PubMed
“… In recent years, psoriasis itself has been recognized as a series of systemic inflammatory diseases, and that the cytokines involved can induce a variety of other diseases.” This report attempts to “unravel the objective data on psoriasis and its complications from various reviews and reports, and introduce the impact of biologics, which are currently the main treatment for psoriasis, on cardiac vascular disease.”
Which Therapy for Which Patient: Psoriasis Comorbidities and Preferred Systemic Agents | PubMed
“The past decade has seen a paradigm shift in our understanding of the pathogenesis of psoriasis that has led to identification of new therapeutic targets. Several new drugs have gained approval … but still a large number of patients continue to be untreated or undertreated.” This article “focuses on specific comorbidities and provides insights to choose appropriate systemic treatment in patients with moderate to severe psoriasis.”

Related Medical Calculators
Psoriasis Area and Severity Index (PASI)
Treatment of Psoriatic Arthritis