DERMATOLOGY
A Practical Guide for Managing Testosterone-Induced Acne in Transgender Patients
Clinical Review Summaries and Resources
Sign up for Figure 1 and be notified directly of new clinical cases and related research, CME activities, quizzes, news, and trends. It’s free!
Figure 1, 2 ,3

Acne is a common and unsettling adverse effect of gender-affirming testosterone treatment

Mild to moderate acne can be managed by topicals and/or oral antibiotics; severe acne often requires oral isotretinoin
A multidisciplinary approach can increase the likelihood of treatment success and prevent unwanted side effects
Transgender people undergoing hormone therapy with testosterone commonly experience acne as an unwanted side effect. Acne does not just affect the skin; it can worsen body image and cause mental distress. Patients receiving testosterone will most likely experience acne; therefore, it is essential for healthcare professionals (HCPs) to become familiar with the treatment of testosterone-induced acne.
Acne vulgaris is a common skin condition that represents the second highest cause of disability from skin diseases globally. Acne pathogenesis is multifactorial, including hormones, inflammation, bacteria, and skin turnover dysfunction. Hormonal acne is caused by the overproduction of sebum from androgens such as testosterone and dihydrotestosterone (DHT). Clinically, hormonal acne tends to affect areas with high sebum production, such as the chest, back, and upper arms. Exogenous testosterone therapy is indicated for transmasculine patients as part of their gender-affirming hormone therapy. Although there is no evidence-based guideline on managing testosterone-induced acne, the current recommendations are extrapolated from cisgender people not receiving testosterone.
Managing Testosterone-Induced Acne in Transgender Patients Clinical Review Summaries and Resources
Initial Evaluation
The initial evaluation of acne for all patients requires proper history taking, with particular attention to whether the patient can or cannot become pregnant. Some acne treatments have teratogenic potential; thus, the HCP needs to determine whether the patient can become pregnant. For example, transmasculine patients with a functional uterus and ovaries have become pregnant, regardless of testosterone therapy status. On the other hand, those who underwent hysterectomy and/or bilateral oophorectomy could not become pregnant. Those who can become pregnant should be on contraceptives or remain abstinent while taking medications with teratogenic potential.
The iPLEDGE program is a safety program to manage the risk of isotretinoin’s teratogenicity and to minimize fetal exposure. A recent change to iPLEDGE includes incorporating more gender-neutral language for those who can and cannot become pregnant. If the patient has a functional uterus and ovaries, then the patient is enrolled under “patient who can get pregnant,” and contraception must be considered.
Grading Acne Severity
The physician global assessment is commonly used to grade acne severity. Mild acne consists of some comedones and no more than a few inflammatory papules and/or pustules. Moderate acne has some inflammatory papules and/or pustules and no more than one nodule. Severe acne has more than one nodule, plus the inflammatory papules and/or pustules. It is vital to examine the patient’s trunk (chest and back), in addition to the face. As mentioned earlier, testosterone-induced acne favors the trunk.
Treatment Options
For mild acne, topical treatments may suffice. The three main treatments are benzoyl peroxide, antibiotics, and retinoids. For moderate to severe acne, oral antibiotics, hormonal contraceptives, and isotretinoin should be considered.
Topical Retinoids
All acne patients should be on topical retinoids; the topical retinoids include adapalene, tretinoin, tazarotene, and trifarotene. Trifarotene is the only topical retinoid approved for truncal acne.
While all topical retinoids have the risk for teratogenicity, the known teratogenic effects of tazarotene should be emphasized. Patient education on topical retinoid use and its side effects are paramount to ensure medication compliance and treatment success.
Common topical retinoid application pearls:
- Wash the face with gentle skin cleanser.
- Apply a pea-sized amount of the retinoid to the cheeks, chin, and forehead every other night for the first four weeks.
- Apply a non-comedogenic nighttime moisturizer.
Mild skin irritation and scaling are common side effects. If the side effect persists, patients can use the short contact method in which topical retinoid is washed off after 30-60 minutes for the first month.
Benzoyl Peroxide and Topical Antibiotics
Topical benzoyl peroxide (BPO) and topical antibiotics (clindamycin or erythromycin) are used to treat mild to moderate acne. To reduce the risk of antibiotic resistance, topical antibiotics should not be used for more than three months and should always be combined with topical BPO.
Oral Antibiotics
This is indicated for moderate to severe acne or acne involving larger surface areas such as truncal acne. Oral doxycycline and minocycline are usually first-line options. Oral erythromycin, azithromycin, amoxicillin, and trimethoprim-sulfamethoxazole are alternatives. Doxycycline and trimethoprim-sulfamethoxazole are teratogenic and potentially teratogenic, respectively, and contraception should be considered. Oral antibiotics are usually prescribed for no more than three months, and if the patient requires more than three months, then isotretinoin should be strongly considered.
Oral Spironolactone
Spironolactone is a mineralocorticoid antagonist and has moderate anti-androgen effects. This medication is highly effective for cisgender women and transfeminine patients. Still, for the transmasculine patients receiving testosterone, spironolactone may not be advisable since it blocks the masculinizing effects of testosterone and may cause unwanted side effects (irregular bleeding, breast tenderness, and gynecomastia).
Hormonal Contraceptives
Hormonal contraceptives (HC) are best managed by the hormone physician in a multidisciplinary setting. Transmasculine patients may avoid HC due to concerns of potential feminizing effects, spontaneous bleeding, and unwanted side effects such as weight gain and breast tenderness. A discussion with the patient’s hormone physician is warranted if the patient is eligible for oral antibiotics and/or isotretinoin — this is to address contraception and the teratogenic risks of antibiotics and isotretinoin.
Isotretinoin
Oral isotretinoin is indicated for severe recalcitrant acne, treatment-refractory moderate acne, or acne that causes significant scarring or psychosocial distress. Patients who can become pregnant must receive monthly contraceptive counseling, monthly pregnancy monitoring and commit to either complete abstinence with men and those assigned male at birth, or consistent use of two forms of contraception. The concerning side effects of isotretinoin in transmasculine patients are listed below.
Potential Side Effects of Treatment
Effects on Mood
Controversies exist on whether isotretinoin causes depression, mood changes, anxiety, and suicidality. Definitive causation has not been established. Since transgender individuals have a higher prevalence of mental health diagnoses than cisgender people, it is essential to screen and monitor for signs of depression in transmasculine patients receiving isotretinoin.
Effects on the Liver and Lipids
Isotretinoin hepatotoxicity and hypertriglyceridemia effects should be routinely monitored via liver function tests and lipid panels. Theoretically, testosterone and isotretinoin can amplify hepatotoxicity effects; therefore, it is imperative to obtain labs at baseline, one month post-initiation of isotretinoin, and the month after dose escalation.
Delayed Wound Healing
Since isotretinoin can delay wound healing for six to 12 months after therapy completion, patients should avoid gender-affirming surgeries for up to a year after stopping isotretinoin.
Summary
Testosterone-induced acne is common and can negatively impact the quality of life of transgender people receiving the therapy. As multiple acne medications may be teratogenic, physicians should thoroughly assess the possibility of a patient becoming pregnant.
A multidisciplinary approach, which includes the dermatologist, primary care or hormone physician, gender-affirming surgeon, reproductive health, and mental health specialists, is essential for successfully managing acne in transgender people receiving testosterone.
Acne Patient Cases
Click on the image to see the full case details and sign in to view community comments.
See more cases like these
Sign up for Figure 1 and gain access to a library of 100,000+ real-world cases.

Continuing Medical Education
How to Talk with Transgender Patients in Primary Care: Learn to better communicate with transgender patients to provide complex and comprehensive care. Start free CME activity >
Free Dermatology CME
Sign up for Figure 1 and gain access to our continuously growing CME & Education Center full of visually interesting and unique CME activities.

References
Lee G, Ferri-Huerta R, Greenberg KB, Somers KE. Acne fulminans in a transgender boy after an increase in testosterone dosage. JAAD Case Rep. 2022;21:32-34. Published 2022 Jan 6. doi:10.1016/j.jdcr.2021.11.029
Radi R, Gold S, Acosta JP, Barron J, Yeung H. Treating Acne in Transgender Persons Receiving Testosterone: A Practical Guide. Am J Clin Dermatol. 2022;23(2):219-229. doi:10.1007/s40257-021-00665-w
Turrion-Merino L, Urech-García-de-la-Vega M, Miguel-Gomez L, Harto-Castaño A, Jaen-Olasolo P. Severe Acne in Female-to-Male Transgender Patients. JAMA Dermatol. 2015;151(11):1260-1261. doi:10.1001/jamadermatol.2015.0761
Wanta JW, Niforatos JD, Durbak E, Viguera A, Altinay M. Mental Health Diagnoses Among Transgender Patients in the Clinical Setting: An All-Payer Electronic Health Record Study. Transgend Health. 2019 Nov 1;4(1):313-315. doi: 10.1089/trgh.2019.0029. PMID: 31701012; PMCID: PMC6830528.
Additional Resources
LGBTQ Advocacy Resources for Physicians | American Medical Association
“The AMA is helping to build a more just, more equitable, more diverse health care system for physicians and patients alike. We advocate at the state and federal levels for quality evidence-based health care regardless of gender or sexual orientation. The AMA is working to advance health equity so all people can achieve optimal health and will continue to strongly oppose discrimination based on an individual’s sex, sexual orientation or gender identity.”
LGBTQI+ Health & Well-being | U.S. Department of Health and Human Services; Office of Population Affairs
“HHS works to ensure that LGBTQI+ people, their families, and communities receive equal access to health services by providing enhanced resources for LGBTQI+ health issues; developing better information regarding LGBTQI+ health needs; and working to close the LGBTQI+ health disparities gap that currently exists.”
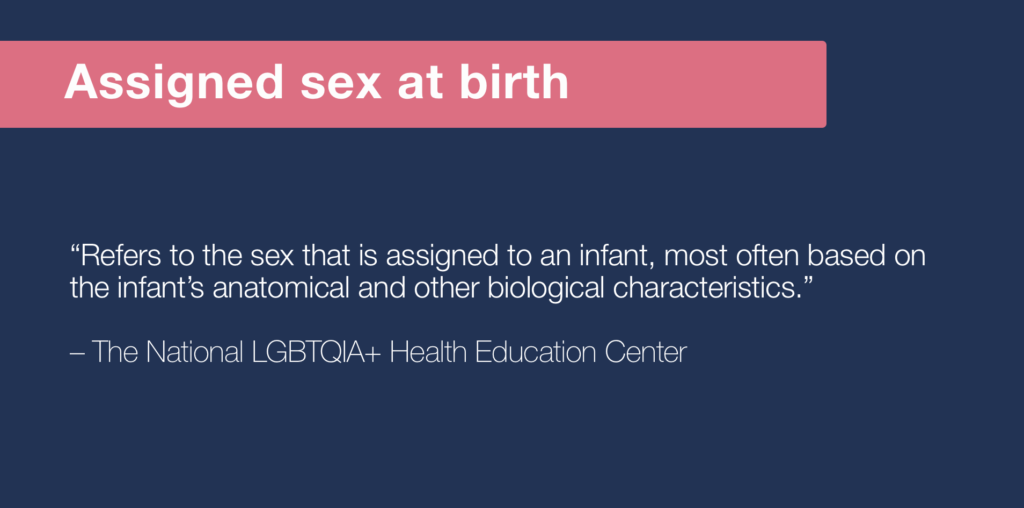
The National LGBTQIA+ Health Education Center
“We provide educational programs, resources, and consultation to health care organizations with the goal of optimizing quality, cost-effective health care for lesbian, gay, bisexual, transgender, queer, intersex, asexual, and all sexual and gender minority (LGBTQIA+) people.”

Benny Wu, DO, PhD
Assistant Professor, Division of Dermatology; Director, Inpatient Dermatology, Albert Einstein College of Medicine/Montefiore Medical Center