One-Sentence Research Summaries
1. In patients with newly diagnosed mIDH1 AML (median age, 76 years), ivosidenib monotherapy achieved median overall survival of 12.6 months. Read the study
2. The benefit of gemtuzumab ozogamicin in non-CBF AML patients with favorable or intermediate ELN 2017 risk is restricted to those with signaling mutations. Read the study
3. A loss-of-function polymorphism in IL6R reduces risk of JAK2V617F mutation and myeloproliferative neoplasm, supporting inflammation as an independent risk factor for JAK2V617F mutation and myeloproliferative neoplasm. Read the study
4. The American Society of Clinical Oncology (ASCO) announced its support for drug repository programs, to help reduce the nearly $3 billion that is lost annually to cancer drug waste, with the condition that they will be for oral medications maintained within a closed system. Read the article
5. What to do when your grant is rejected. Read the article
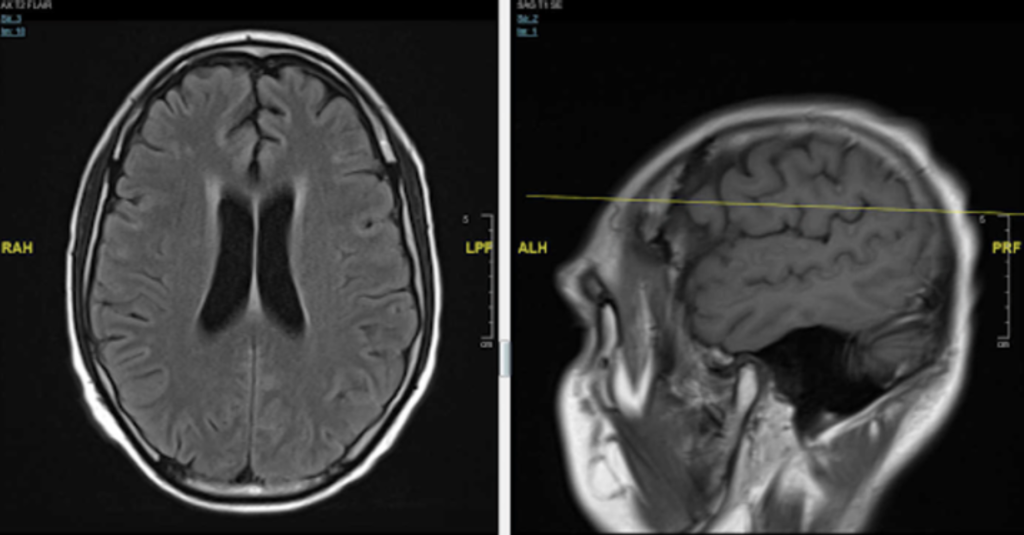
CNS Relapse in AML: In Case You Missed It
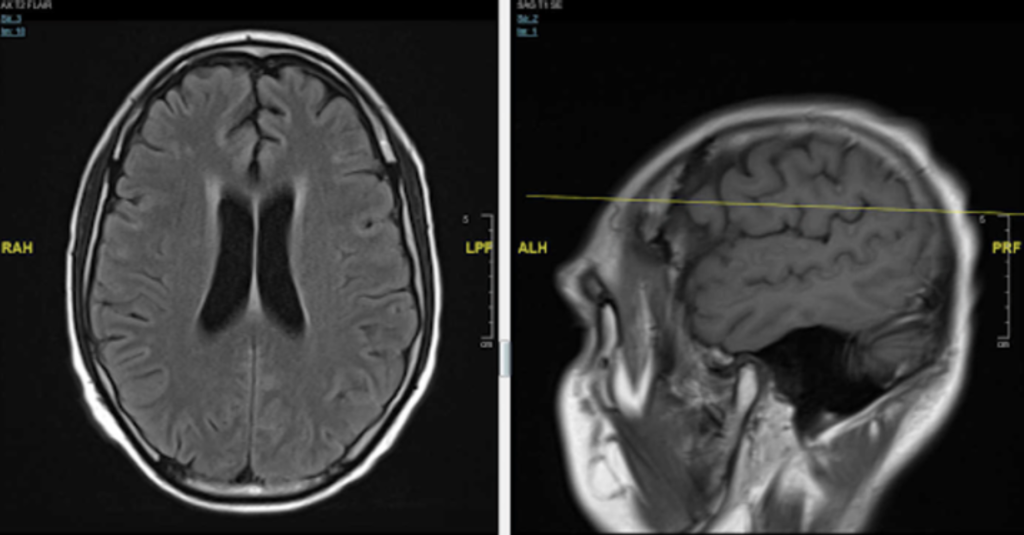
This 26-year-old was diagnosed with CNS relapse of AML three years ago
He initially presented with leukocytosis and fevers, the karyotype was der(1;7)(q10;p10), and next-generation sequencing showed mutation in KRAS codon 12. He was treated with conventional induction chemotherapy with daunorubicin 90 mg/m2/d x 3 and cytarabine 100 mg/m2/d x 7, and achieved remission. He then underwent transplant.
A year ago, he developed headaches, fatigue, and nausea. His blood counts were normal. On exam, there was no evidence of leukemia cutis or focal neurological deficits. Marrow biopsy was normal with full donor chimerism. CSF showed an increased WBC count with 77% blasts that are positive for CD45(dim), CD13, CD15 and CD56(dim), and very dim for CD117. He was treated with intrathecal chemotherapy serially until clearance for CNS relapse, followed by donor lymphocyte infusion. Recurrence of CNS symptoms and abnormal cytology led to treatment with high-dose cytarabine, then radiation, and then high-dose methotrexate, then nivolumab on a clinical trial. He now presents with another CNS recurrence.
What would you do next?
Narrative Medicine
When the Teenager or Young Adult Has Cancer
Adolescents and young adults are a special population of cancer patients.
“My patient was brought to the emergency room by his friend because he could no longer catch his breath and had a cough that wouldn’t extinguish. He lived with three other young men, all in their early 20s, in a small house located in what many of us considered the no-man’s land between Cleveland and Buffalo, the four of them suspended between spending some time in a community college and finding work that they might one day call a career…”
Read the full essay in The New York Times

By Mikkael Sekeres, MD, MS
Chief of the Division of Hematology, Sylvester Comprehensive Cancer Center, University of Miami Miller School of Medicine
Originally published March 5, 2020
Join the Conversation
Register for Figure 1 and be part of a global community of healthcare professionals gaining medical knowledge, securely sharing real patient cases, and improving outcomes.


