NEUROLOGY
Preventing Stroke in Symptomatic Intracranial Atherosclerotic Arterial Stenosis
Practice Advisory and Resources
Sign up for Figure 1 and be notified directly of new clinical cases and related research, quizzes, news, and trends.

Figure 1, 2 ,3
In severe sICAS, clopidogrel should be added to aspirin for up to 90 days for long-term prevention of stroke and death

sICAS patients should have a goal LDL < 70 mg/dL and a long-term blood pressure target of <140/90

No recommendation for percutaneous transluminal angioplasty and stenting, angioplasty alone, direct bypass, or surgical revascularization for stroke prevention in patients with sICAS
Summary
Symptomatic intracranial atherosclerotic arterial stenosis, or sICAS, is a common cause of stroke, accounting for 10–50% of strokes worldwide. In March 2022, the American Academy of Neurology published a practice advisory for the management of sICAS. These guidelines are also endorsed by the American Heart Association and American Stroke Association, the Neurocritical Care Society, and the Society of Vascular and Interventional Neurology.
These recommendations are based on results of clinical trials, including: Warfarin-Aspirin Symptomatic Intracranial Disease trial (WASID), Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis trial (SAMMPRIS), Clopidogrel Plus Aspirin versus Aspirin Alone for Reducing Embolisation in Patients with Acute Symptomatic Cerebral or Carotid Artery Stenosis trial (CLAIR), Clopidogrel and Aspirin for Reduction of Emboli in Symptomatic Carotid Stenosis trial (CARESS), Clopidogrel in High-risk Patients with Acute Nondisabling Cerebrovascular Events trial (CHANCE), Trial of Cilostazol in Symptomatic Intracranial Arterial Stenosis (TOSS).
Atopic Dermatitis Comorbidities Clinical Guidelines and Resources
Key Findings
- All patients with stroke should be assessed for symptomatic intracranial atherosclerotic arterial stenosis using diagnostic modalities such as CT angiography or magnetic resonance angiography.
- sICAS should be treated with aspirin 325 mg/day over warfarin for long-term prevention of stroke and death. Clopidogrel 75 mg/day should be added to aspirin for up to 90 days in those with severe (70–99%) sICAS and low risk of hemorrhagic transformation of ischemic stroke. Cilostazol 200 mg/day is a reasonable alternative to clopidogrel 75 mg/day.
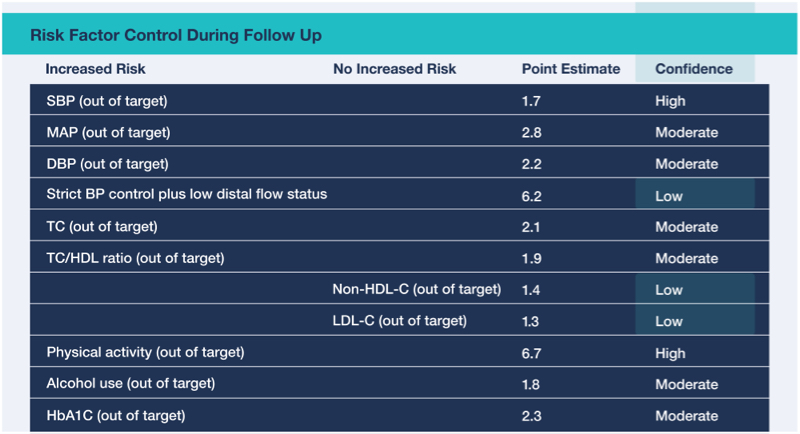
- To reduce risk of recurrent stroke and vascular events, symptomatic intracranial atherosclerotic arterial stenosis patients are recommended to be on a high-intensity statin therapy to achieve a goal LDL < 70 mg/dL and to have a long-term blood pressure target of <140/90.
- Moderate physical activity is recommended in patients with sICAS who are safely capable of exercise to reduce the risk of recurrent stroke and vascular events.
- Treatment of modifiable vascular risk factors is recommended in patients with symptomatic intracranial atherosclerotic arterial stenosis to reduce the risk of recurrent stroke and vascular events.
- There is no consensus recommendation for bilateral arm ischemic preconditioning (BAIPC) in patients with sICAS. The available studies had small sample sizes and were not blinded. While the risk of the procedure appears low, the BAIPC device does not have approval for use in the United States.
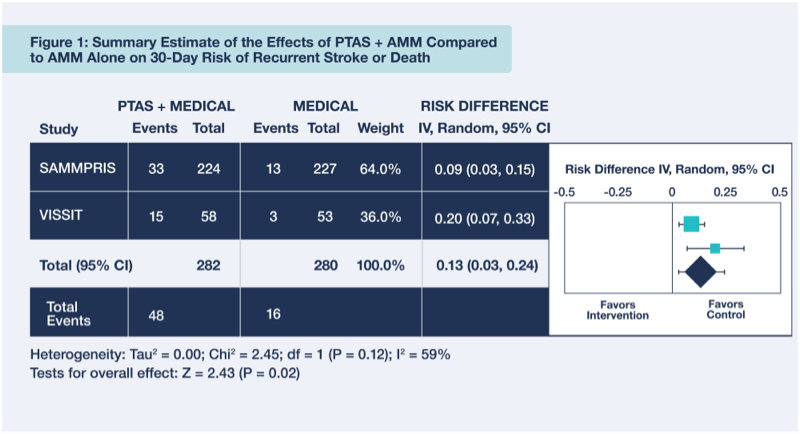
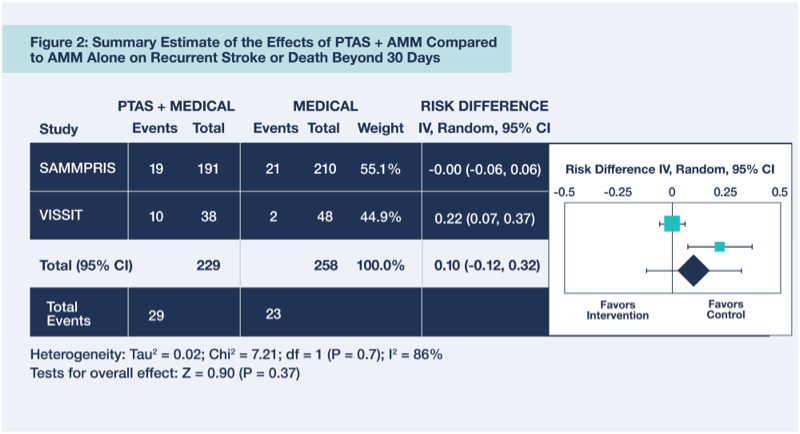
- Percutaneous transluminal angioplasty and stenting (PTAS) is not recommended as the initial treatment for stroke prevention in patients with sICAS, based on several randomized trials that showed no benefit.
- Angioplasty alone is not recommended for stroke prevention in patients with symptomatic intracranial atherosclerotic arterial stenosis given the lack of efficacy data.
- Direct bypass is not recommended for stroke prevention in patients with sICAS due to lack of established efficacy.
- Indirect surgical revascularization is not recommended for stroke prevention in patients with sICAS due to lack of established efficacy.

Full Practice Advisory
Read the full practice advisory from AAN: Stroke Prevention in Symptomatic Large Artery Intracranial Atherosclerosis Practice Advisory
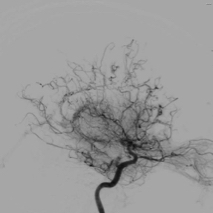
Summary Estimate of the Effects of PTAS + AMM Compared to AMM Alone on Recurrent Stroke or Death
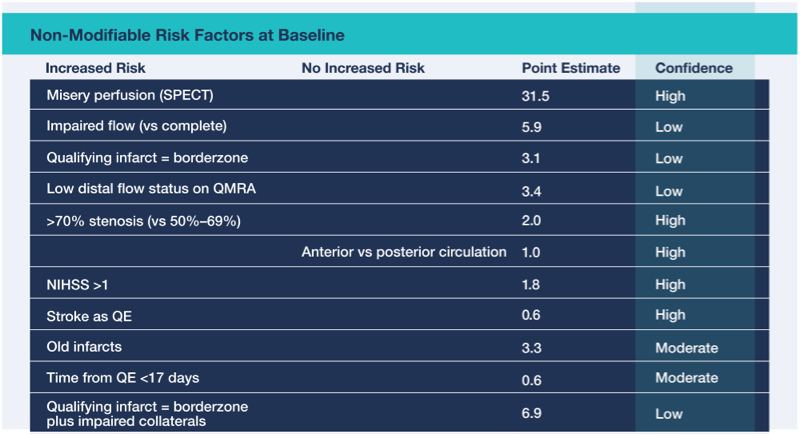
Predictors of Recurrent Stroke or Death in Patients With sICAS

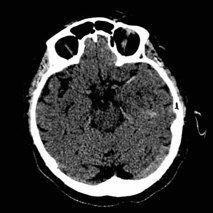
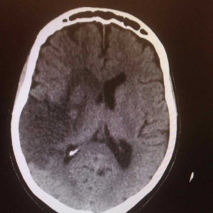
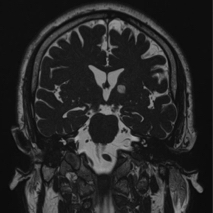
Stroke Patient Cases
Click on the image to see the full case details and sign in to view community comments.
See more cases like these
Sign up for Figure 1 and gain access to a library of 100,000+ real-world cases.


Related Research
“There is no consensus on the optimal treatment for acute ischemic stroke (AIS) large vessel occlusions (LVOs) or near-occlusions with underlying intracranial atherosclerotic stenosis (ICAS). We report the first American series using intra-arterial (IA) glycoprotein IIb/IIIa inhibitors (GPIs) as a stand-alone revascularization technique for ICAS presenting with large vessel ischemic syndromes … results highlight the utility of IA GPI administration as the first-line therapy for symptomatic ICAS near occlusions or as a rescue technique after failed thrombectomy for LVO patients suspected of underlying ICAS.”
“To date, few clinical studies have investigated the effect of serum bilirubin on symptomatic intracranial atherosclerotic stenosis (sICAS). This study aims to evaluate the connection between serum bilirubin and sICAS … the logistic regression analyses showed that lower levels of Tbil, Dbil, and Ibil were related to multiple (≥3) atherosclerotic stenoses (95% CI: 2.365-5.298 in tertile 1 and 2.312-5.208 in tertile 2 for Tbil; 1.743-3.835 in tertile 1 and 1.416-3.144 in tertile 2 for Dbil; 2.361-5.345 in tertile 1 and 1.604-3.545 in tertile 2 for Ibil) when compared with tertile 3 … findings suggest that lower bilirubin levels may indicate severe and multiple intracranial atherosclerotic stenoses.”

Related Medical Calculators
Modified NIH Stroke Scale/Score (mNIHSS)
Rapid Arterial Occlusion Evaluation (RACE) Scale for Stroke