Pathophysiology
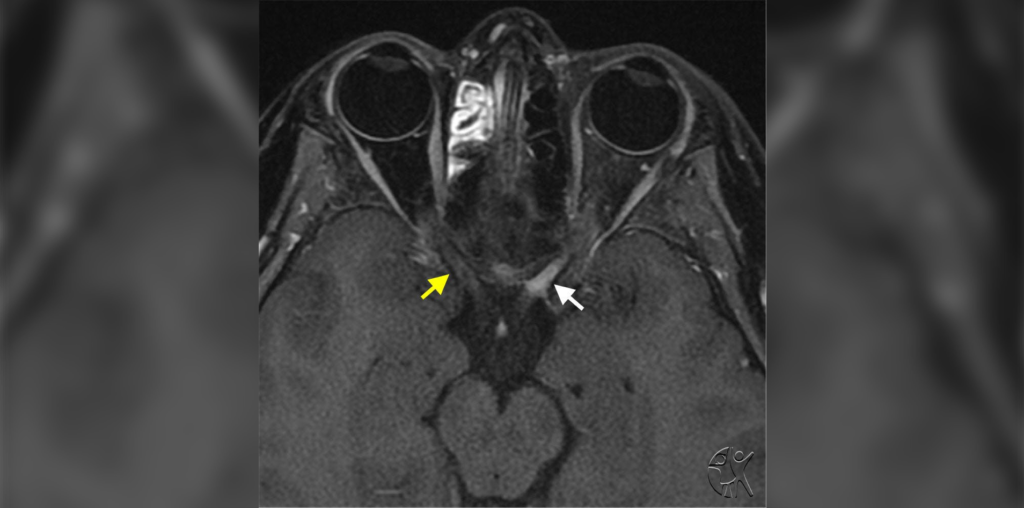
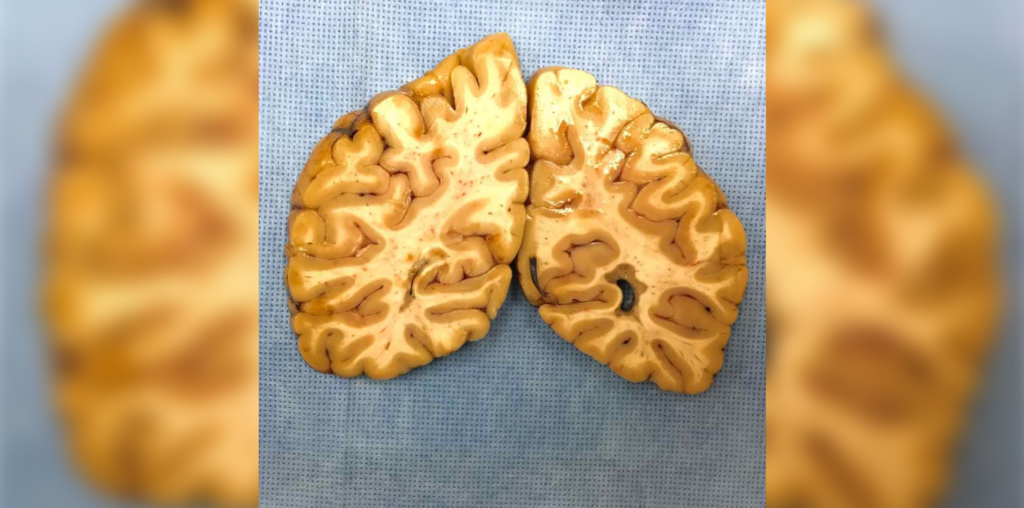
Multiple sclerosis, or MS, is an autoimmune disease affecting the central nervous system. This presents most often as demyelinating lesions in the brain and spinal cord.
Epidemiology
The mean age of onset is 20-30 years old. Environmental, lifestyle, and genetic factors are thought to contribute to the disease. For instance, multiple sclerosis is more prevalent at higher latitudes, suggesting an association with lower vitamin D levels. The disease is also more prevalent within families and is associated with the HLA-DR1*15:01 allele. Childhood obesity, cigarette smoking, and Epstein-Barr virus are also associated with the development of MS.
Clinical Presentation
Classic presentations of multiple sclerosis include unilateral optic neuritis, intranuclear ophthalmoplegia, vertigo, myelitis, and focal sensory or motor changes.
Multiple Sclerosis Diagnosis
The diagnosis of MS is based on the McDonald Criteria, which was last revised in 2017. The diagnosis is defined by dissemination of multiple sclerosis characteristics in space and time. Dissemination in space refers to the distribution of lesions in the central nervous system, including infratentorial, juxtacortical, cortical, periventricular, and spinal cord. Dissemination in time refers to the development of new lesions over time.
The revised McDonald Criteria made the following changes: “in patients with a typical clinically isolated syndrome and clinical or MRI demonstration of dissemination in space, the presence of CSF-specific oligoclonal bands allows a diagnosis of MS; symptomatic lesions can be used to demonstrate dissemination in space or time in patients with supratentorial, infratentorial, or spinal cord syndrome; and cortical lesions can be used to demonstrate dissemination in space.”
Relapse Treatment
For relapses that impair function, treatment typically consists of high-dose steroids, for instance, intravenous methylprednisone at a dose of 500-1000 mg for three to five days.
Disease Modifying Treatment
Disease modifying therapy (DMT) for multiple sclerosis aims to prevent the accumulation of disability. Injectable DMTs (interferons, glatiramer acetate) reduce relapse rates by 29-34% compared with placebo. Oral DMTs (fumarates, teriflunomide, S1P modulators) reduce relapse rates by 36-58%. Monoclonal antibody infusions (natalizumab, ocrelizumab, alemtuzumab) have the highest efficacy and reduce relapse rates by 68% compared to placebo. However, these infusions tend to have a higher incidence of serious adverse reactions. For instance, alemtuzumab is associated with autoimmune conditions and natalizumab is associated with progressive multifocal leukoencephalopathy.
Ponesimod is one of the newest DMTs and was approved in March 2021 for relapsing forms of multiple sclerosis. It is an oral medication taken daily and has been shown to reduce annual relapse rates and reduce disease activity on MRI compared to treatment with teriflunomide, an approved DMT. In February 2021, the U.S. Food & Drug Administration approved a new intramuscular injection route of administration for peginterferon beta-1a, a DMT for relapsing forms of MS.
Multiple Sclerosis Treatment Strategy
There are two main treatment strategies. One approach is to start with the least potent medications with fewer side effects and escalate when there is evidence of disease activity on imaging or exam. This approach minimizes the risks of side effects but can potentially result in more accumulated disability. A second treatment approach is to start with a high efficacy medication to provide better disease control. However, this approach can expose patients to a higher risk of adverse events. Currently, there is no standard recommended approach.
Pregnancy and Breastfeeding
Women are often diagnosed with multiple sclerosis during their childbearing years. Relapse rates tend to be lower during the first and third trimesters of pregnancy compared with the year prior to pregnancy. All DMTs except glatiramer acetate should be discontinued at least four months prior to conception. Steroids for acute exacerbations should be avoided during the first trimester of pregnancy. With the possible exception of the injectable DMTs, breastfeeding is not recommended while on DMTs.
Symptomatic Treatment
Multiple sclerosis is associated with disabling symptoms, including spasticity, pain, fatigue, cognitive impairment, bladder and bowel dysfunction, and mood disorders. A team of health care professionals can provide multidisciplinary support to achieve comprehensive care.

By Joy Lin, MD
Neurologist
Published April 6, 2022
Join the Conversation
Register for Figure 1 and be part of a global community of healthcare professionals gaining medical knowledge, securely sharing real patient cases, and improving outcomes.