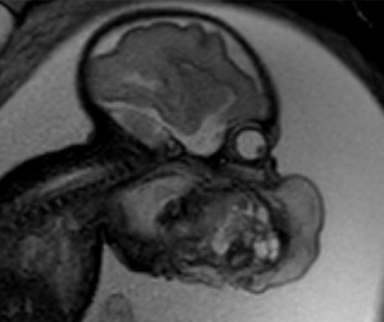
“An 87-year-old male with a history of stroke presents with a skin lesion that first appeared 3 months ago. The patient has been in nursing-home care for 18 months and has not received any further treatment. Lesion measures 2 cm and is asymmetrical, deep red/purple in colour, and is on the left side of the the face. Symptoms include further loss of mental agility and as well as speech ability.”
This case was shared by a medical student on Figure 1, and the community began to discuss the best next steps for management.
The first comments are clear: This patient would be better left alone without unnecessary procedures.
“He’s 87 and in poor mental and physical health. His time is limited. This needs to be seriously considered before putting him through a procedure that will cause pain and stress. Will it extend or improve anything with his health/life? Likely not. Let him be in peace.”
Nursing Assistant
“Doesn’t say it is bothering him. Any procedure would. And worse, he likely wouldn’t be able to understand what was happening. Sounds like he is in sharp decline regardless. No treatment is going to help this man. How about you go in and hold his hand and talk for 5 minutes every day to him? Way more therapeutic benefit than anything else would be now to him.”
Nursing Assistant
Others disagree, stating that treatment, or at the very least a biopsy, is ethical and necessary.
“Why do you assume a biopsy equates to unnecessary treatment? There are ways to manage CA [carcinoma] that would not be to the patient’s detriment. But, before any of those can be considered, first a dx [diagnosis] is needed.”
Family Medicine Physician
“It’s not bothering him… yet. Are we going to wait until it’s a big fungating and suppurating mass on his face, or are we going to make a dx and then decide what’s best for him? Without a dx we have no options because we don’t know what we’re dealing with. Just leaving it would be substandard care.”
Family Medicine Physician
“If a biopsy can be performed and a malignancy proven, it may be less distressing for the patient and his relatives to have a short course of radiation therapy. Of course, this would be subject to any advanced health directive or family requests.”
Registered Nurse
“In my opinion it is unethical to simply let this go. Minimally it needs biopsy. Then decide what potential Tx (treatments) are possible. This looks more like melanoma to me. He could live long enough for this to become a real problem for him.”
Paramedic
Of course, these decisions aren’t easy. Some physicians expressed the need to involve family members before making any choices.
“I partly agree. I would nonetheless biopsy for a diagnosis. If SCC/BCC [squamous cell carcinoma/basal cell carcinoma] can consider palliative XRT [radiotherapy] vs other options. As long as the patient is fully informed including the different treatment options (surgery radiation, topical chemo, observation). These tumors are usually not fatal but can cause significant morbidity due to their location in the head and neck.”
Head and Neck Surgery Resident
“There is a middle ground between biopsy then surgery, and doing nothing. You could treat it with Efudex, and if it becomes inflamed, you will have a diagnosis of SCC/BCC, and if he tolerates it, it would be at least palliative. The family should be part of the decision-making process.”
Dermatologist
What do you think would be the best next course of action? What would you and your colleagues decide?
Published September 21, 2021; updated July 2022
Join the Conversation
Register for Figure 1 and be part of a global community of healthcare professionals gaining medical knowledge, securely sharing real patient cases, and improving outcomes.