Learning Objectives
- Recognize the clinical presentation of gelastic seizures
- Describe the most common cause of gelastic seizures
A 6-year-old with no notable health history presents to a psychologist for frequent inappropriate outbursts of uncontrollable laughter and unprompted aggressive behavior toward other children. The patient is taller than expected for their age and has prominent acne. The psychologist recommends behavioral therapy and gives a referral to endocrinology to be evaluated for precocious puberty.
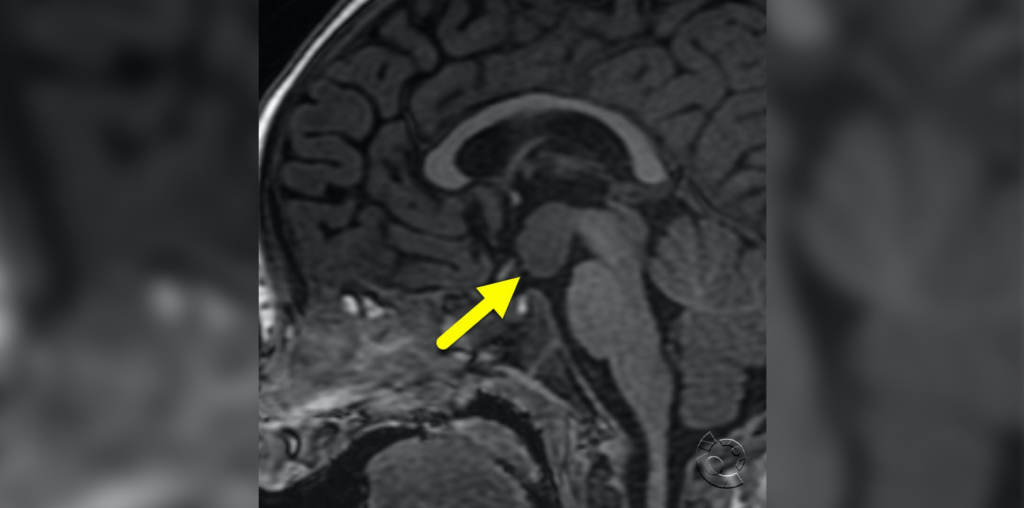
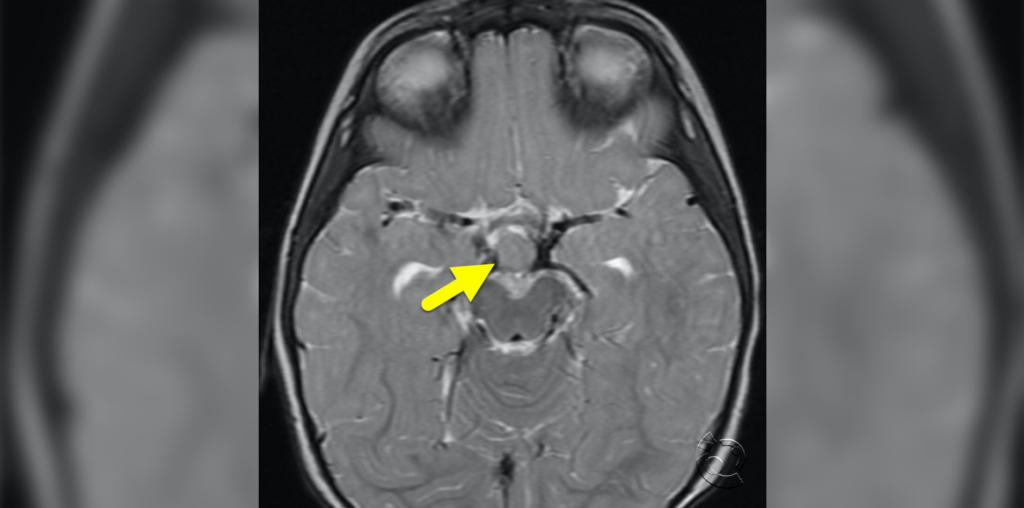
Subsequent MRI shows a hypothalamic hamartoma. Upon learning about the laughter, the endocrinologist is concerned about gelastic seizures which are confirmed by ictal EEG.
Gelastic seizures are brief (less than 30 seconds) fits of unprompted, unsuppressable laughter or forced smiling classified as focal non-motor emotional seizures. Although conventionally the laughter is described as “mirthless,” some patients may have an associated sensation of joy. Gelastic seizures may be isolated or embedded in other symptoms like automatisms or staring spells.
Onset is typically in infancy but frequently goes unrecognized for years. Patients often develop other seizure types as they age, including dacrystic (crying or grimacing), tonic, atonia, or generalized tonic-clonic seizures. These are nearly always medically refractory, requiring surgical intervention. The spectrum of associated symptoms is broad, and may or may not include cognitive disability, behavioral and psychiatric issues such as rage, or developmental regression. Endocrine abnormalities (specifically central precocious puberty) are present in up to half of symptomatic patients with hypothalamic hamartomas.
Hypothalamic hamartomas (HH) are rare benign congenital lesions which are closely associated with gelastic seizures. Because of the depth of the epileptogenic focus, surface EEGs are at risk of missing isolated gelastic seizures. Even on imaging, HH may be extremely small and difficult to identify, putting patients at high risk of misdiagnosis without a high degree of clinical suspicion. 3D volumetric 3 Tesla MRI is the preferred imaging method when available. More recently, extra-hypothalamic foci of gelastic seizures have been recognized as well, particularly in the frontal or temporal lobes.
Further Reading
Hypothalamic Hamartoma With Epilepsy: Review of Endocrine Comorbidity
Mechanisms of Intrinsic Epileptogenesis in Human Gelastic Seizures with Hypothalamic Hamartoma
References
Demir AB, Öz BY, Yıldız MO, Türk BG, Tanrıverdi T, Bekar A, Yeni N, Bora İ. A clinical evaluation of gelastic and dacrystic seizures: a multicenter study. Arq Neuropsiquiatr. 2022 Dec;80(12):1204-1212. doi: 10.1055/s-0042-1758755. Epub 2022 Dec 29. PMID: 36580957; PMCID: PMC9800159.
Nathan T. Cohen, J. Helen Cross, Alexis Arzimanoglou, Samuel F. Berkovic, John F. Kerrigan, Ilene Penn Miller, Erica Webster, Lisa Soeby, Arthur Cukiert, Dale K. Hesdorffer, Barbara L. Kroner, Clifford B. Saper, Andreas Schulze-Bonhage, William D. Gaillard, on behalf of the Hypothalamic Hamartoma Writing Group. Hypothalamic Hamartomas: Evolving Understanding and Management. Neurology Nov 2021, 97 (18) 864-873; DOI: 10.1212/WNL.0000000000012773
Striano S, Meo R, Bilo L, Cirillo S, Nocerino C, Ruosi P, Striano P, Estraneo A. Gelastic epilepsy: symptomatic and cryptogenic cases. Epilepsia. 1999 Mar;40(3):294-302. doi: 10.1111/j.1528-1157.1999.tb00707.x. PMID: 10080508.

Kaci McCleary, MD
Hospice and Palliative Care Fellow, OhioHealth
Published April 19, 2023
Want more clinical cases?
Join Figure 1 for free and start securely collaborating with other verified healthcare professionals on more than 100,000 real-world medical cases just like this one.