Learning Objective
- Understand the cause and characteristics of shiitake dermatitis
You’re at your shift in the emergency department, when a 50-year-old arrives complaining of a new skin eruption. They say the rash developed suddenly over the past two days and describe it as “a bit itchy,” but are most concerned by the way the rash appears: long linear welts clustered together. The first cluster developed on the chest, followed by another on the back. As you take a health history, you find nothing remarkable. The patient mentions recently eating at an Asian food festival, although they have eaten similar foods before and never had a reaction.
Vitals and Physical Exam
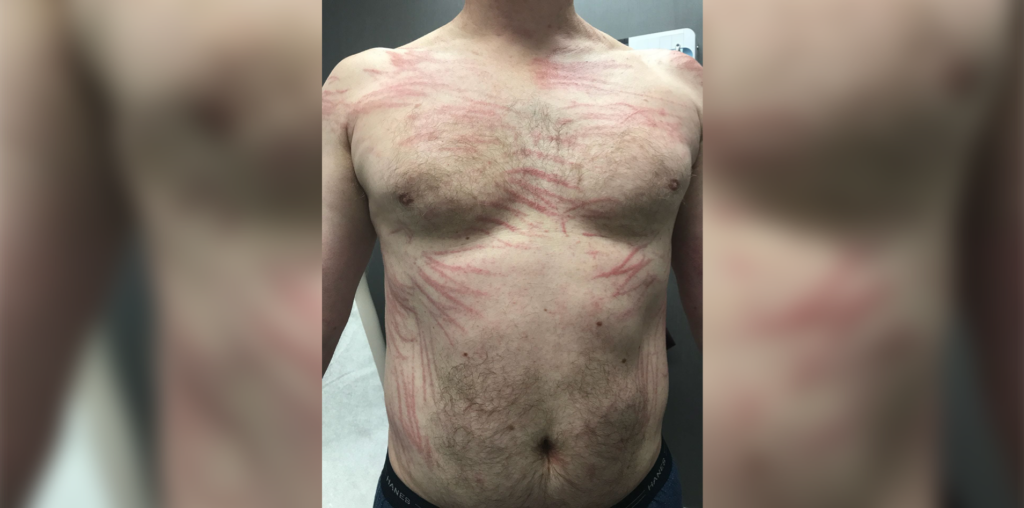
On examination, there are no systemic signs. Vital signs are normal and aside from the lesions, there appears to be no signs of any chronic skin disease. The lesions themselves are linear, occasionally crossing the midline, as well as crossing dermatomes. They also are mildly edemitous. It looks like dermatographism. As a quick test, you scratch the skin, and nothing appears in that location. The skin is dry, and there isn’t any weeping or discharge.
You follow up by asking a few more questions about atopy, but the patient has no allergies: not to foods, environments, or medications.
The patient has shiitake dermatitis, a particular type of food-associated dermatitis. These lesions are described as “flagellate,” which is another way of saying they look like whiplash, and is why this is also referred to as shiitake flagellate dermatitis.
Pathology
The lesions are caused by a compound present in shiitake mushrooms called lentinan. In a few papers, Lentinan has been described as activating certain types of leukocytes. This compound has been isolated and tested as a form of chemotherapy for some types of gastrointestinal cancer in Japan, where cases of flagellate dermatitis have been described as a side effect of treatment.
When thoroughly cooked, lentinan is degraded by heat, reducing the risk of dermatitis to most shiitake mushroom lovers. However, consuming raw or undercooked mushrooms, containing the still-active lentinan, can initiate a cutaneous inflammatory response.
Diagnosis and Treatment
The characteristic linear rash develops within two days of exposure, and the diagnosis is often clinical, based on history and examination findings. The condition is self-limiting, typically resolving within three weeks, though it can recur with repeat exposure. Management is supportive, and treatment with oral corticosteroids is unnecessary.
Differential Diagnosis
There have been case reports of shiitake dermatitis presenting with linear collections of vesicles in a dermatomal distribution. So, the differential diagnosis includes an atypical presentation of herpes zoster, allergic dermatitis, or drug eruption. The presence of fever, lymphadenopathy, severe pain, or edema should raise suspicion of another diagnosis, including drug reaction with eosinophilia and systemic symptoms, or DRESS for short.

By Kyle Slinn, RN, BScN, MEd
Registered Nurse
Further Reading
References
Adler MJ, Larsen WG. Clinical variability of shiitake dermatitis. J Am Acad Dermatol. 2011;67(4):e140–e141.
Baran W, Batycka-Baran A, Maj J, Szepietowski JC. Shiitake dermatitis – now also in Poland. Acta Derm Venereol. 2015 Jan;95(1):102-3.
Garg S, Cockayne SE. Shiitake dermatitis diagnosed after 16 years! Arch Dermatol. 2008 Sep;144(9):1241-2.
Hamer S, Rabindranathnambi R. A wide-spread flagellate dermatitis. BMJ Case Rep. 2013;Jan 3:2013: bcr2012007682.
Karanovic S, George S, Topham E. Don’t miss shiitake dermatitis: a case report. Br J Gen Pract. 2014 Aug; 64(625): 426–427.
You read the case. Now get free CME credit.
Sign up for Figure 1— it’s free! — and earn CME credit based on this clinical case. You’ll also gain access to our expanding CME & Education Center full of unique CME activities just like this one.