Learning Objectives
- Identify features of posterior cortical atrophy on MRI
- Recognize posterior cortical atrophy as a potential presentation of Alzheimer disease
- Appreciate the role of ancillary tests in diagnosing atypical presentations of Alzheimer disease
A 72-year-old, left-handed, cis woman is referred to the neurology clinic for complaints of difficulty reading. She describes difficulty reading certain specific types of text, which she first noticed about one year ago. She can read a similar news item in one newspaper but not in another. She saw an optometrist, who found no issues with her glasses prescription. Both the patient and the referring family physician worried that her unusual symptoms were psychogenic.
With a more detailed interview, it becomes evident that the issue is not the size but the style of lettering. She can easily read plain texts, but when more elaborate flourishes are added (as with certain styles of newspaper headings), she has trouble discerning both individual letters and entire words. There are no other neurological symptoms such as visual blurring, visual field defects, visual agnosia (i.e., no difficulty recognizing objects, faces, colors, etc.), memory loss, behavior or personality changes, hallucinations, sleep disturbances, seizures, abnormal movements, or falls.
Her neurological examination shows difficulties with the visuospatial portion of the Montreal Cognitive Assessment (trail-making, cube and clock drawing) scoring 25/30 in total. Reading aloud various samples of text confirms there is no surface or phonological alexia, no issues with language production or comprehension, and no simultagnosia; plain text styles are read normally no matter how large/small, including nonsense syllables or words with irregular spelling (e.g., yacht). She easily recognizes and names objects and describes the details and overall representation of various photographs and paintings. The rest of the neurological examination is normal.
Simultanagnosia refers to the loss of ability to perceive more than one item at a time, with patients typically seeing the individual details of pictures but not the whole. This is attributed to an impaired visual attention or inability to scan and perceive the “big picture.” A related concept is that of apperceptive visual agnosia. Whereas this patient did not have trouble perceiving objects, her inability to see the words or letters formed by the individually perceived dashes, dots, or flourishes of complicated fonts, could perhaps be called a “lexical” simultanagnosia. The specificity of the complaint and the consistency of the findings on examination — including a non-amnestic, visuospatial pattern of cognitive impairment — were highly suspicious for a neurological cause for her symptoms.
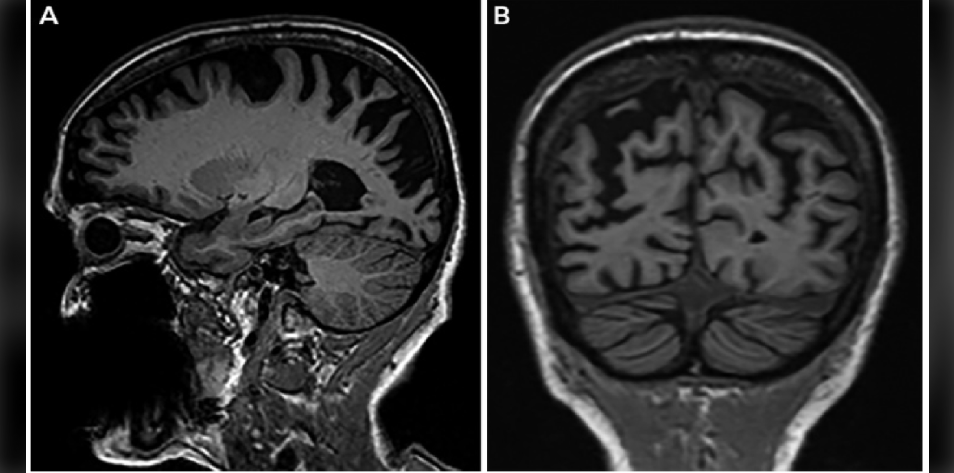
MRI brain (image 1) shows prominent asymmetric cortical atrophy predominantly affecting the posterior temporal, parietal, and occipital lobes — a pattern consistent with posterior cortical atrophy (PCA), a neurodegenerative syndrome that presents with various visuospatial or perceptive difficulties. Patients often go through a long and convoluted process to get to an accurate diagnosis, due to a delay in considering a neurological cause for their atypical visual symptoms. The two most common underlying causes of PCA are Alzheimer disease and Lewy body disease (LBD). In more rapidly progressive cases, the Heidenhain variant of Creutzfeldt-Jakob disease is also an important consideration.
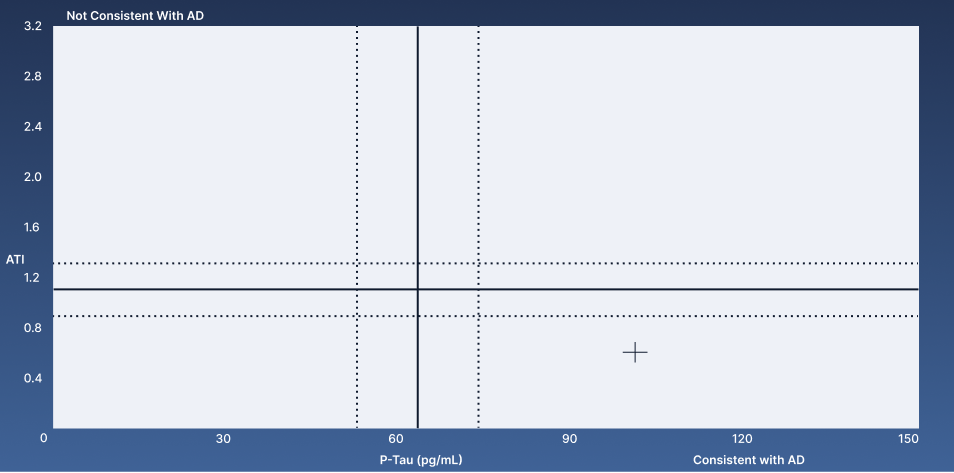
Alzheimer disease can be differentiated from LBD using ancillary tests like functional neuroimaging (positron emission tomography or single-photon emission computed tomography) or cerebrospinal fluid testing for Alzheimer disease markers, namely tau and amyloid. Lumbar puncture is performed, and the patient’s results (image 2 — indicated by a cross) showed an elevated phosphorylated tau (p-tau) and a decreased amyloid-tau index (ATI) — a pattern consistent with Alzheimer disease.
The patient is given various suggestions to adapt her home environment and daily activities to compensate for her visual challenges. Working with occupational therapy can be highly beneficial. In subsequent years, as the visuospatial dysfunction begins interfering with instrumental activities of daily living, patients are also offered symptomatic treatment with acetylcholinesterase inhibitors.
PCA is an important atypical presentation of Alzheimer disease. Accurate diagnosis is crucial to provide diagnostic closure and appropriate support for patients.
Further Reading
Consensus Classification of Posterior Cortical Atrophy
References
Schott JM, Crutch SJ. Posterior Cortical Atrophy. Continuum (Minneap Minn) 2019;25(1):52-75.
Graff-Redford J, Yong KXX, Apostolova LG, et al. New insights into atypical Alzheimer’s disease in the era of biomarkers. Lancet Neurol 2021;20(3):222-234.

Aravind Ganesh, MD, DPhil(Oxon), FRCPC
Vascular and Cognitive Neurologist and Assistant Professor, University of Calgary Department of Clinical Neurosciences
Published September 21, 2022
Want more clinical cases?
Join Figure 1 for free and start securely collaborating with other verified healthcare professionals on more than 100,000 real-world medical cases just like this one.