A 36-year-old presents to the emergency department with two days of vomiting preceded by three months of supine headaches. When asked, they endorse baseline blurry vision that has worsened. Their father and a cousin both died from renal cell carcinoma in their 40s.
On exam, the patient has bilaterally decreased visual acuity, left arm ataxia, and wide based gait. Fundoscopic exam shows bilateral papilledema and peripheral capillary proliferation.
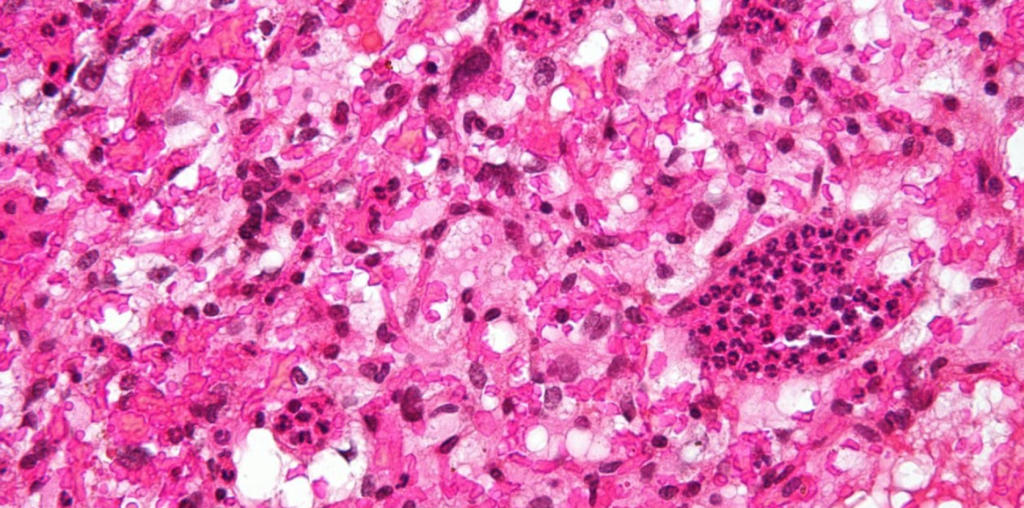
Brain imaging reveals a cystic infratentorial mass, and abdominal CT shows several cysts throughout the abdominal cavity. They are taken for urgent resection of the brain lesion. Histologically, it shows hyperchromic, pleomorphic mesoderm-derived stromal cells filled with lipids and glycogen and enmeshed in a dense vascular network (representative slide shown).
The patient is diagnosed with hemangioblastoma related to von Hippel-Lindau (VHL) disease, an autosomal dominant disorder caused by mutation in the VHL tumor suppressor gene. It is classically characterized by retinal angiomas, cerebellar hemangioblastomas and clear cell renal carcinoma. Treatment includes mass resection and radio- or cryoablation. Surveillance may be appropriate for pre-symptomatic lesions.
Further Reading
Von Hippel-Lindau Disease: Current Challenges and Future Prospects
References
Maher, E., Neumann, H. & Richard, S. von Hippel–Lindau disease: A clinical and scientific review. Eur J Hum Genet 19, 617–623 (2011). https://doi.org/10.1038/ejhg.2010.175
Lonser, Russell R, Glenn, Gladys M, Walther, McClellan, Chew, Emily Y, Libutti, Steven K, Linehan, W Marston, & Oldfield, Edward H. (2003). Von Hippel-Lindau disease. The Lancet (British Edition), 361(9374), 2059-2067.

Kaci McCleary, MD
Hospice and Palliative Care Fellow, OhioHealth
Published March 29, 2022
Want more clinical cases?
Join Figure 1 for free and start securely collaborating with other verified healthcare professionals on more than 100,000 real-world medical cases just like this one.