Quick Medical Quizzes to Test Your Knowledge
Challenge yourself with Figure 1’s medical quizzes.

Medical quizzes on Figure 1 provide a quick, fun way for healthcare professionals to test their knowledge.
Our popular quizzes provide a learning lift for our members and offer a competitive challenge — all based on real patient cases shared on Figure 1.
How Our Qbank Works
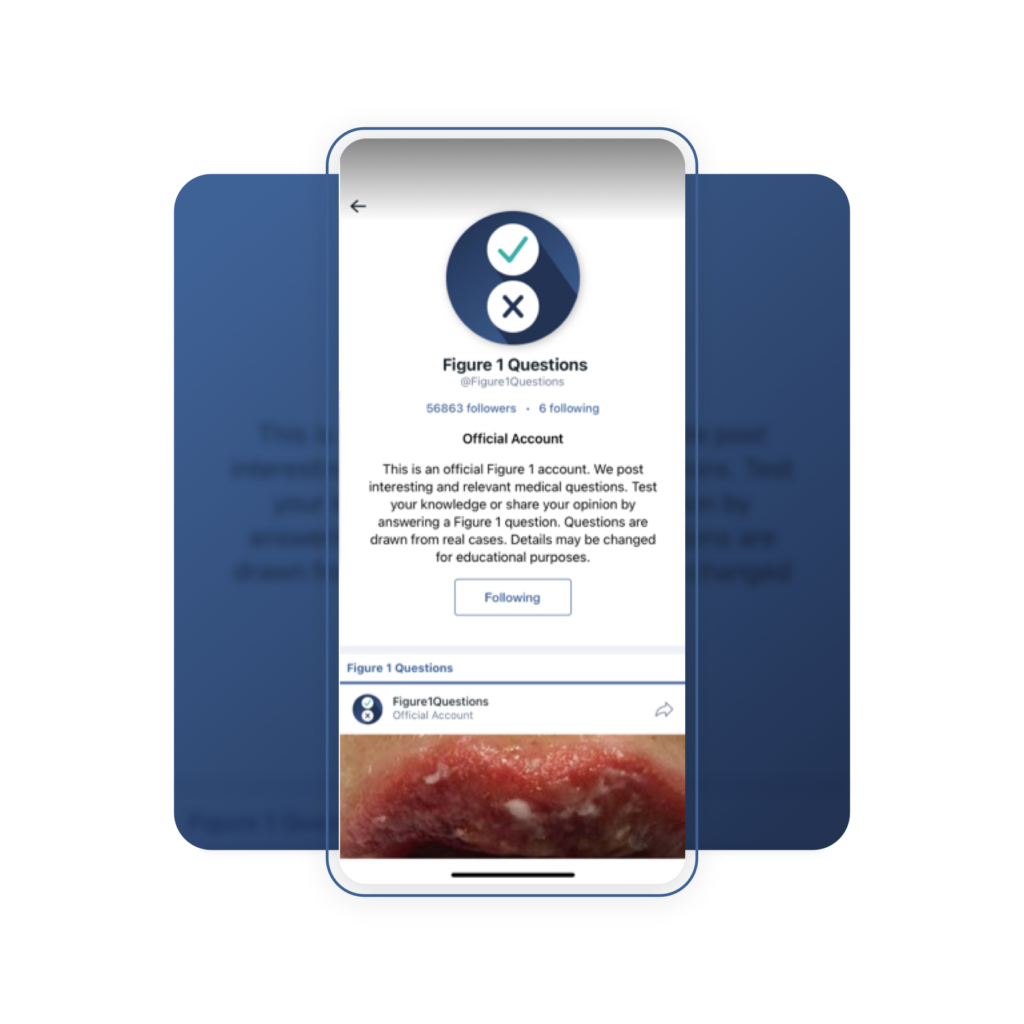
Medical quizzes are published weekly to our Figure1Questions official account on the Figure 1 platform. Each quiz is flagged by a banner that says Quick Quiz.

How to Take a Quiz
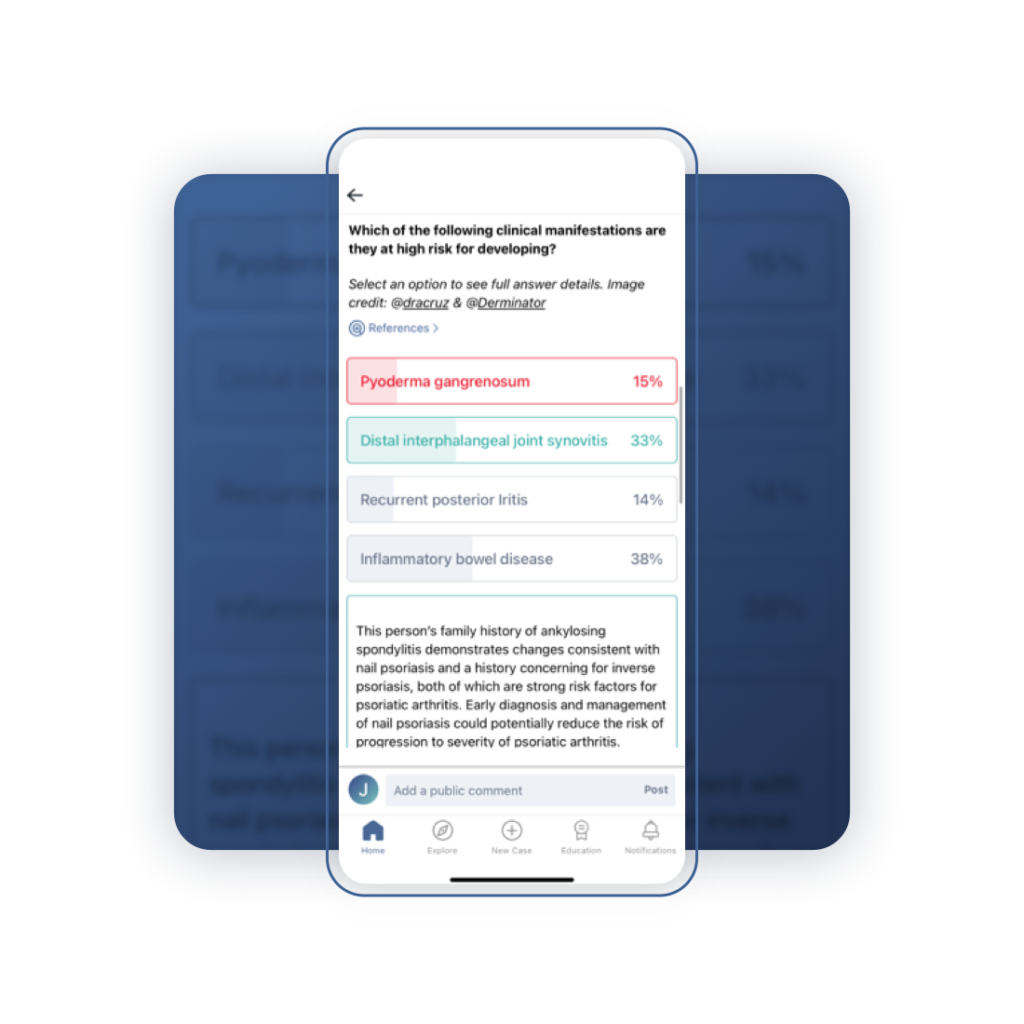
At the bottom of the case description is a multiple-choice question. Simply click on the option you believe is correct. When you do, you will see the correct answer, what percentage of members chose which option, and an explanation behind the right and wrong answers.
Real Patients, Real Cases, Real Discussions
Real-Life Cases
The quizzes are derived from real-life cases shared on Figure 1, which means they generally test the same questions that real members request from one another: some ask about the correct diagnosis, while others focus on the best potential strategies for care.
Real Feedback
Each medical quiz also has a comment section, which provides an opportunity for healthcare professionals to share their feedback and thoughts on the quiz, and capture nuanced aspects of the case or share further knowledge from their experiences with similar cases.
Convenient Learning
At Figure 1, we know that healthcare professionals are extremely busy, all the time. That’s why we offer these quick medical quizzes in a number of different channels, so that you can access them whenever you are in the right frame of mind to acquire a bite-sized piece of medical knowledge.
On the Platform …
The quizzes appear in the Figure 1 feed, in the Figure1Questions account, and in the Quizzes+ feed on the platform. As you are browsing cases on your device of choice (iOS, Android, or web browser) if you notice a post by the username Figure1Questions, that is our official account for posting medical questions. To make sure you see the quizzes as they are posted, follow the Figure1Questions account.
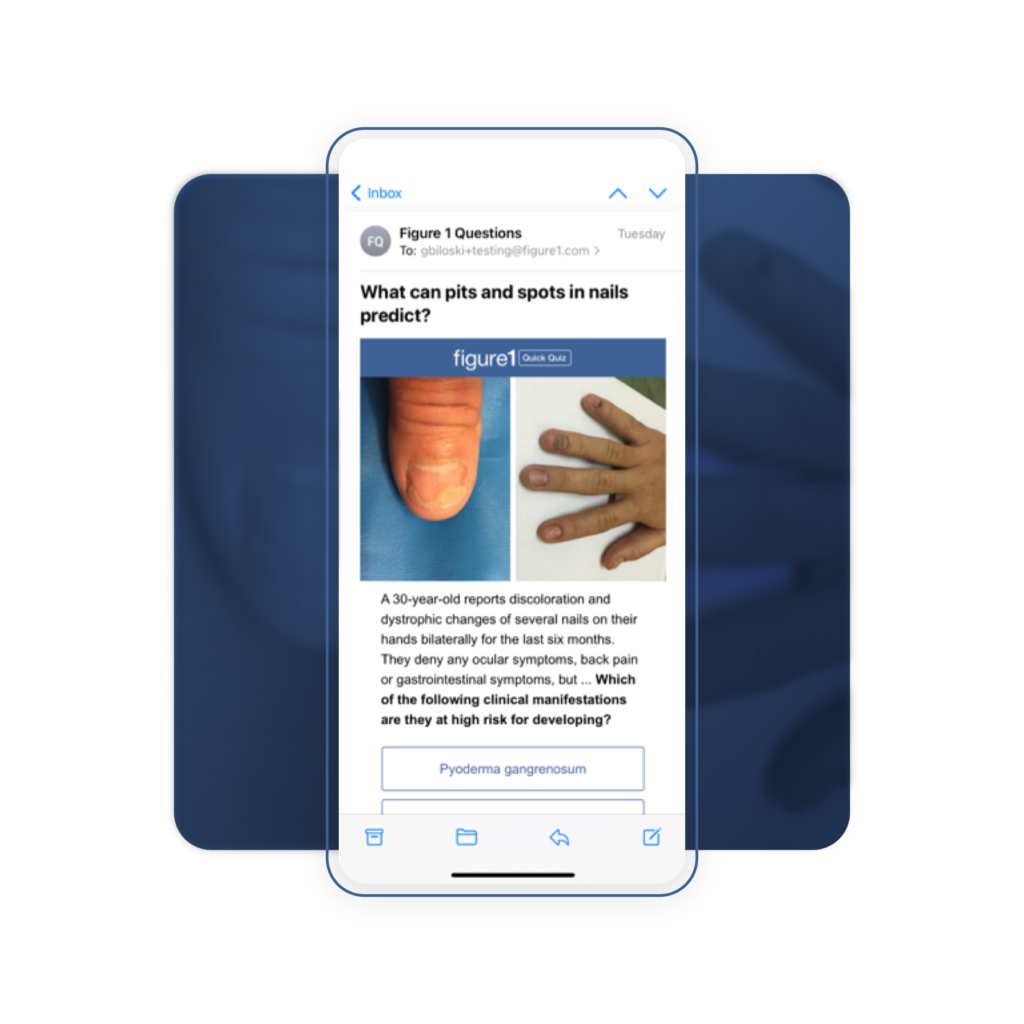
… and Delivered to Your Inbox
We also regularly email questions to our members, so you’ll be alerted to a new quiz right from your inbox.



