Learning Objectives
- Understand the link between COVID-19 mRNA vaccines and myocarditis
- Explain to patients the risk associated with COVID-19 mRNA vaccines and myocarditis
In November of 2021, a 14-year-old in Incheon, South Korea began to complain of headaches. They visit their local clinic, and are given medication to help with the pain. A week later, while exercising, they suddenly faint. They are taken to a nearby hospital and after some imaging and blood tests, the healthcare team discovers the patient has developed myocarditis.
The team looks for possible causes, but can’t find anything. The only notable finding is that 12 days before the fainting episode, they received the first dose of the Pfizer COVID-19 vaccine.
There have been a few stories like this — cases of myocarditis caused by the mRNA COVID-19 vaccines. Most of the reported cases happened in cis-men under the age of 30.
Academic literature investigating these cases is now being published and we’re getting a glimpse into how likely people are to develop the disease from the mRNA COVID-19 vaccines, and how severe their symptoms tend to be.
Research Overview
In December 2021, the American Heart Association published a retrospective study looking at patients under the age of 21 years who experienced myocarditis within 30 days of receiving an mRNA COVID-19 vaccine. Here’s some of the key points from that study.
The researchers chose patients diagnosed with the disease and patients suspected of having the disease coupled with elevated troponin levels or abnormal cardiac function. The median age of the selected 139 participants was 16 years, the majority of which were assigned male at birth and white. Almost everyone in the study experienced myocarditis after their second vaccine dose.
For these patients, symptoms began within a week of either their first or second vaccine dose, with a median of two days. They all experienced chest pain, a third of them had a fever, and a quarter experienced shortness of breath.
Most of them had abnormal ECGs, but only a handful had non-sustained ventricular tachycardia. A fifth of the patients developed left ventricular ejection fractions of less than 55%, which resolved for them all. And for those who received a cardiac MRI scan, both gadolinium enhancement and myocardial edema were seen on their imaging.
The median hospital stay for these patients was two days, but ranged anywhere from zero to 10 days. Eighteen percent of them went to the ICU for care.
So how did the healthcare teams treat these patients? Well, most were treated with NSAIDs, although the researchers of this study weren’t able to determine if NSAIDs were given for pain management or for anti-inflammatory reasons. About a fifth of patients received IVIG and/or glucocorticoids, and only two people received inotropic support. And finally, about a tenth of patients received no treatment at all.
Takeaways
So what are the takeaways here? First, yes, there does appear to be a link between myocarditis and the mRNA vaccines, but it is extremely rare.
So, let’s put this into perspective. In the United States, the chances of being killed in a car crash, from drowning, or from choking on food far outweigh the chance of developing myocarditis from the mRNA COVID-19 vaccine.
In fact, people have a one in 625 chance to develop myocarditis by being infected by COVID-19. That’s a rate 16 times higher than developing myocarditis from the vaccine.
Now, while this study looked at primarily patients who took the Pfizer COVID-19 vaccine, there’s emerging evidence that suggests the Moderna vaccine has a very slightly higher risk of causing the disease. Again, not by much, but a higher risk nonetheless. This has led some public health agencies to prioritize giving the Pfizer vaccine to people under 30.
And as a point of comparison, here’s the likelihood someone under 30 would develop the disease in 2021, without having COVID-19 or getting the vaccine.
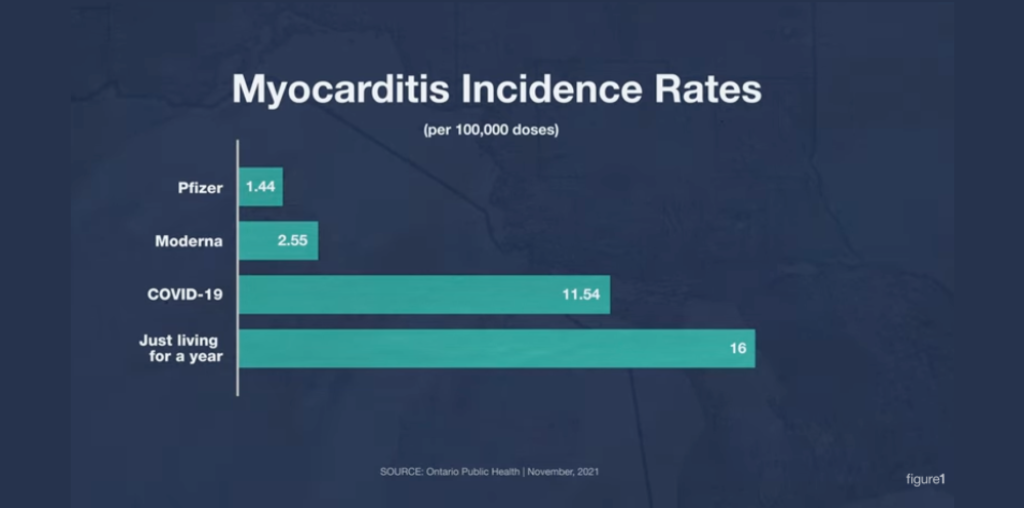
And for those who noticed these numbers are different from the numbers shared previously, it’s because these numbers were pulled from a different study, which had different sample sizes and took place at a different time in 2021. The key point here is myocarditis from the vaccine is really low, in both cases.
This data for the most part lines up well with some of the initial studies we saw previously.
“In the USA, 296 million doses of these MRNA vaccines have been given, [through] June this year. And of these there were 1,226 reports of myocarditis after vaccination. In the U.S. they clumped myocarditis, pericarditis, and myopericarditis under the term myocarditis … In those patients the median age of those people who were affected was 26 years, and the time to onset was a median of three days after vaccination.”
Here’s another takeaway: myocarditis caused by the vaccines is almost always mild. Patients recovered quickly, had short hospital stays, and they all survived. Most hospitalizations were primarily for observation, with patients receiving little to no treatment at all, which is pretty similar to previous findings.
“Now there was an analysis of the patients in the U.S. and they found that 96% of those patients who had myocarditis had to be hospitalized, but fortunately there were no deaths. In the European economic area, five deaths have been reported from myocarditis caused by vaccination, however these are generally older patients who had more comorbidities. The general consensus is the prognosis is good, however we do not have enough data over a longer period of time to understand if there are any longer-term issues.”
As more information has continued to be uncovered, public health agencies have begun recommending patients that do develop myocarditis from the vaccine not receive additional doses.
Conclusion
Should patients be worried about myocarditis caused by mRNA vaccines? No. The risk is incredibly small.
If patients are vaccine hesitant, ask them if they’d like to discuss the personal barriers they are facing and help them to better understand vaccine risks and benefits.

By Kyle Slinn, RN, BScN, MEd
Registered Nurse
Want more clinical cases?
Join Figure 1 for free and start securely collaborating with other verified healthcare professionals on more than 100,000 real-world medical cases just like this one.