Summary
Following a normal first trimester, a pregnant patient starts spotting. The patient’s care provider books an urgent ultrasound to see what is causing the bleeding. The main concerns are if the spotting is caused by a miscarriage or something else.
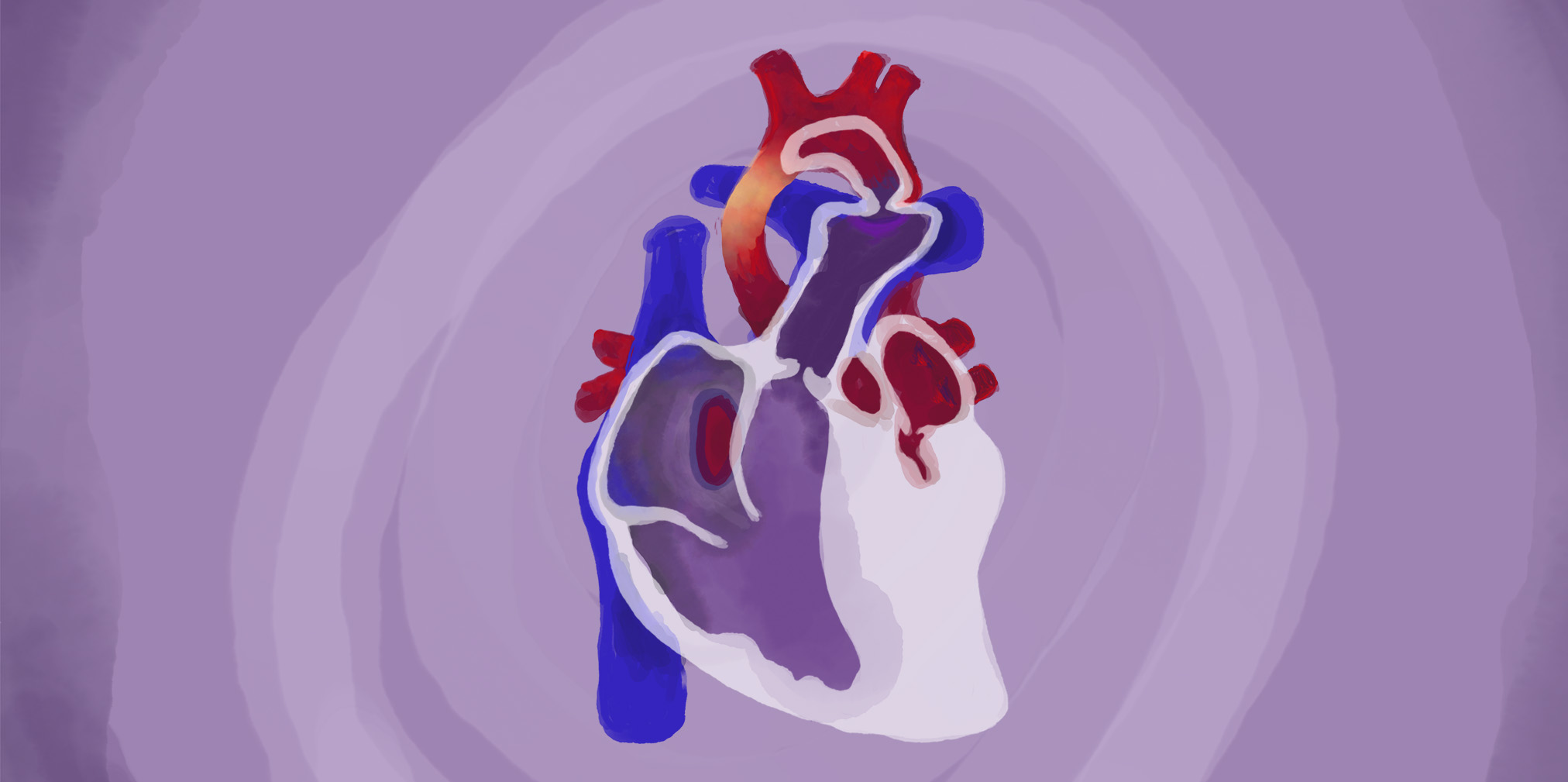
Following the ultrasound, the technician calls obstetrician, Dr. Ashley Brant, to review the results with the patient. There is a problem with the fetus’ heart — specifically, a condition called hypoplastic left heart syndrome. Essentially, the left side of the heart doesn’t develop normally and can’t pump blood in the way that it should.
Hypoplastic left heart syndrome causes poor oxygenation, meaning the skin can be bluish or with dark discolorations. It also causes difficulty breathing, feeding, and lethargy. Treatment includes multiple surgeries after birth, and can even require a heart transplant.
Without treatment, the condition is fatal.
The patient is offered genetic testing to determine if the heart condition is a symptom of a larger genetic disease. Regardless, the prognosis is grim.
The patient meets with Dr. Brant to discuss all of the options, including continuing or ending the pregnancy.
“I think everybody who’s in a situation where they’re thinking about ending a pregnancy because of a major fetal anomaly, they are thinking about what is the kindest decision, the most loving decision that they can make for their baby,” shared Dr. Brant. “Nobody wants to be in this position. And they’re thinking about what the experience is going to be like for this child.”
The patient makes the decision to end the pregnancy through the dilation and evacuation method.
However, the procedure cannot be performed in the state because of a heartbeat law in place at the time.
And so Dr. Brant refers the patient to an out-of-state clinic where the initial procedure to stop the heartbeat can be performed. But, in order to be where the patient has the support of the medical team she knows and who has been by her side, the patient returns to her home state for the final procedure.
“No one ever envisions themselves needing an abortion. No one ever thinks, ‘I want to have an abortion,’ before they’re in a position of needing one. I would just encourage compassion and empathy and trying to understand the life that someone else might be walking in.”

Ashley Brant, DO, MPH
Ashley Brant, DO, MPH, is a physician in the Ob/Gyn & Women’s Health Institute at Cleveland Clinic. She is the Director of the Complex Family Planning Program and she co-leads the Pregnancy Early Assessment Clinic.
Dr. Brant is board-certified in obstetrics and gynecology and complex family planning. She is an Assistant Professor of Surgery at the Cleveland Clinic Learner College of Medicine at Case Western Reserve University.
She is active in research on the use of telemedicine in women’s health, contraceptive counseling, postpartum long-acting reversible contraception, contraceptive care service delivery, and the impact of state policies on access to reproductive healthcare.
Transcript
DDx SEASON 7, EPISODE 3
Hypoplastic Left Heart Syndrome and a Trip Across State Lines
Dr. Raj Bhardwaj: This season of DDx is sponsored by Cleveland Clinic. The case studies you’re about to hear are real patient stories. Some details may be changed to preserve confidentiality.
Dr. Ashley Brant: No one ever envisions themselves needing an abortion. No one ever thinks, “I wanna have an abortion,” before they’re in a position of needing one. You know, I would just encourage compassion and empathy and trying to understand the life that someone else might be walking in.
Dr. Bhardwaj: This is DDx, a podcast from Figure 1 about how doctors think.
I’m Dr. Raj Bhardwaj.
This season, we’re doing something different. We’re taking you inside the minds of doctors who perform one of the most essential – and often lifesaving – services in healthcare: abortion.
During this season, you’ll hear from three obstetricians inside Cleveland Clinic.
They’ll tell you about their patients.
Patients whose lives have been saved and emotional health safeguarded by this essential service.
We’ll talk about abortion as it affects physical and mental health.
Today, a case from Dr. Ashley Brant, an Ob/Gyn specialist at Cleveland Clinic in Cleveland, Ohio.
CHAPTER 1 — CASE STUDY
Dr. Brant: This was a young woman who was getting her prenatal care at Cleveland Clinic and throughout her first trimester, everything had gone fine. It was a planned pregnancy and a wanted pregnancy.
Dr. Bhardwaj: But at around 16 weeks, this patient noticed she was spotting.
Dr. Brant: So her healthcare provider helped her get in for an urgent ultrasound to see what was causing the bleeding. Obviously everyone’s first concern is, could this be a miscarriage or, something else serious going on with the pregnancy.
Dr. Bhardwaj: It wasn’t a miscarriage, but there was a serious problem.
Dr. Brant: You can imagine showing up for an urgent ultrasound because you have a gut feeling that something is wrong with the pregnancy. And then, the ultrasound tech, in silence, looking intently at the images on the screen and not giving you any information and calling in the maternal fetal medicine or the high risk OB specialist to go over the results with you. It’s about as intense as any pregnancy experience can get.
Dr. Bhardwaj: The patient was referred to a pediatric cardiologist to talk about the results.
Dr. Brant: They did see that there was a problem with the way that the baby’s heart was developing. So during that ultrasound, they noticed a major fetal cardiac anomaly, something called hypoplastic left heart syndrome.
Dr. Bhardwaj: Hypoplastic left heart syndrome is when the left side of the heart doesn’t develop normally and can’t pump blood the way that it should.
Dr. Brant: And symptoms are what you can expect if you have a baby with left heart hypoplastic syndrome is that the baby doesn’t oxygenate well. They appear cyanotic. Their skin can be bluish colored or they can have dark discoloration of the skin. Difficulty breathing, difficulty feeding, lethargy or low energy. And the symptoms can vary depending on the severity of the anomaly.
Dr. Bhardwaj: Treatment includes multiple surgeries after the baby is born, or a heart transplant. Without treatment this condition is fatal.
Dr. Brant: They were counseled that this cardiac anomaly could be an isolated finding or it could be a part of genetic syndrome, which could have other implications for the baby’s health, and that there was a significant risk that the baby need multiple surgeries after it was born, potentially have a poor quality of life or even possibly experience death in infancy because of the problems with the heart development.
Dr. Bhardwaj: The patient was offered genetic counseling to determine if this heart defect was a symptom of a larger genetic disease. But even if it wasn’t, the prognosis was grim.
Dr. Brant: She met with her maternal fetal medicine specialist, which is her high risk OB specialist, and to talk about all of the options continuing the pregnancy versus ending the pregnancy. I think everybody who’s in a situation where they’re thinking about ending a pregnancy because of a major fetal anomaly, they are thinking about what is the kindest decision, the most loving decision that they can make for their baby. Nobody wants to be in this position. And they’re thinking about what the experience is going to be like for this child.
Undergoing multiple major heart surgeries in the first year of life, the first one potentially within the first week or two of life. What is that recovery gonna be like for a baby? And if there’s still a high risk of the baby not making it, of it dying even after pursuing surgery, some parents would decide that the kindest thing is to end the pregnancy.
Dr. Bhardwaj: During this visit, the patient was counseled on the possibility of ending the pregnancy.
In Ohio, the heartbeat law prohibits most abortions after a fetal heartbeat is detected. It was signed into law in 2019 and was active during this case. It is currently suspended due to a court injunction.
Dr. Brant: And so because of that law, there was a lot of confusion around was it okay to talk about termination as an option? Was it okay to refer patients out of state for termination? And so she’s lucky that her healthcare providers provided the full array of options to her, full intervention surgery continuing the pregnancy to ending the pregnancy and everything in between.
And so after that visit she was counseled about what it would look like to end the pregnancy, in the second trimester, that typically looks like having a surgical procedure, which is called a dilation and evacuation, or having a labor induction. And she was interested in dilation and evacuation.
Dr. Bhardwaj: But because of the heartbeat law, they couldn’t perform that procedure, usually called a “D and E”, at the clinic in Ohio.
Dr. Brant: We couldn’t offer the D and E at our hospital unless the baby had demised, unless the fetal heartbeat had stopped because at that time, abortion was illegal in Ohio, if a fetal heartbeat was present. And so the way that Ohio’s abortion law is written is that it carves out an exception for miscarriage and also for removal of a demised pregnancy of a dead fetus.
Dr. Bhardwaj: So they referred her to a clinic out of state which could perform the procedure.
Dr. Brant: And she inquired about whether it would be possible to come back and have her procedure with us if she could have a procedure out of state to cause the heartbeat to stop.
So that was not something that we had done previously at our hospital. So we worked and collaborated with a clinic in another state to have her get care there to receive an injection that caused the heartbeat to stop. And that allowed her to come back to her healthcare facility where her doctors knew her, where she had gotten all of her care in her hometown in order to have this procedure and to recover from the procedure.
It meant that her partner could be with her on the day of her procedure and that she had family around to help take care of her during her recovery.
Dr. Bhardwaj: The procedure is very safe and the patient recovered well.
But things would have gone much differently if she didn’t have access to this care in the first place.
CHAPTER 2 — LESSONS
Dr. Brant: This patient had a series of things that went right with her care, even though she was in a terrible situation. And that includes being at a healthcare center where her providers could counsel her about all the options.
Her healthcare providers knew who we could refer her to in another state to get the first step in her abortion care. She had the means to be able to take off work, to be able to travel out of state, to be able to pay for her injection in the other state, and then to come back for her procedure with us. You can imagine how. If at any one of those steps she were to encounter barriers, she may have been forced to continue this pregnancy.
Dr. Bhardwaj: For this case, the risks of complications during labor would have increased because of the baby’s high medical needs.
Dr. Brant: Whenever a fetal anomaly is present, there’s also an increased risk of stillbirth, of preterm delivery of complications during the delivery or shortly after the delivery.
There’s the financial impact of caring for a baby with significant medical needs. There’s the psychological impact of caring for a child with significant medical needs, so you can imagine how if at any one of these forks in the road, had she not been able to get her pregnancy termination, her life could be looking very different.
Dr. Bhardwaj: Thanks to Dr. Brant for speaking with us.
This is DDx, a podcast by Figure 1.
Figure 1 is an app that lets doctors share clinical images and knowledge about difficult to diagnose cases.
I’m Dr. Raj Bhardwaj, host and story editor of DDx.
Head over to figure1.com/ddx, where you can find full show notes, photos and speaker bios.
This season of DDx is sponsored by Cleveland Clinic.
Cleveland Clinic is consistently ranked as one of the nation’s top hospitals for gynecologic care, by U.S. News & World Report. Learn more from Cleveland Clinic Women’s Health experts at consult qd dot cleveland clinic dot org.
Thanks for listening!