Summary
A pregnant person is referred early in pregnancy to high-risk obstetrician Dr. Stacey Ehrenberg after an ultrasound detects an abnormally developing placenta. Dr. Ehrenberg diagnoses the patient with a molar pregnancy; a placenta that forms into a benign tumor with the potential to become cancerous. While the molar pregnancy will not survive, the patient also has a viable intrauterine pregnancy.
Faced with this diagnosis, Dr. Ehrenberg counsels her patient about the risks of continuing or discontinuing the pregnancy. If the decision is made to continue, the patient risks developing mirror syndrome, a life-threatening condition marked by hypertension and edema. There is also significant risk of bleeding if any of the abnormal tissue is removed.
If the decision is made to end the pregnancy, the patient faces the risks of any procedure done in a hospital; bleeding, infection, and damage to the surrounding organs, although this happens in less than 1% of cases. Regardless of the patient’s choice, Dr. Ehrenberg emphasizes that she and her team will support the patient, no matter what.
The patient decides to continue the pregnancy. Dr. Ehrenberg and team develop a care plan to track both the molar pregnancy and the intrauterine pregnancy with weekly ultrasounds and blood pressure measurements.
“I really watched her struggle throughout the pregnancy knowing that she knew that at some point the scale was going to tip and that this would no longer be safe for her to continue,” shared Dr. Ehrenberg. “Her hope, as was ours, was that she would be able to get far enough in pregnancy where the baby would be able to survive. She knew that this would probably be an extremely premature baby, but she was willing to take that risk to start her family.”
But at 19 weeks, everything changes.
“I didn’t need vital signs. I didn’t need to do a physical exam to know something wasn’t right,” remembered Dr. Ehrenberg. “We got vital signs on her and I did a physical exam, and it was very clear to me that she had mirror syndrome and then we had to have the very difficult conversation that we knew that the baby was not yet viable, but it was no longer safe for her to remain pregnant.”
The decision is clear: the only viable option is dilation and evacuation.
But the procedure is not without serious complications and risks.
“… These pregnancy complications are so complex,” shared Dr. Ehrenberg. “The physical aspects of it, the emotional aspects of it, the financial aspects of it … So I really just would love to see more kindness towards other people, more tolerance towards other people, more understanding that we don’t understand all the time where other people are coming from and what they’ve been through.”

Stacey Ehrenberg, MD
Stacey Ehrenberg, MD is a maternal-fetal medicine specialist at Cleveland Clinic in Cleveland, Ohio. She specializes in Fetal Therapy and is the Director for Diabetes in Pregnancy for Cleveland Clinic’s Ob/Gyn & Women’s Health Institute.
Dr. Ehrenberg: One of the reasons I became a high risk obstetrician is because I get to know my patients so well. I see them so often that I can look at them and tell something’s not right, and that was the feeling I got that day when she walked in. I took one look at her and she didn’t even have to say anything. I didn’t need vital signs. I didn’t need to do a physical exam to know something wasn’t right.
Transcript
DDx SEASON 7, EPISODE 1
The Complicated Decision-Making of a Molar Pregnancy and an Intrauterine Pregnancy
Dr. Raj Bhardwaj: This is DDx, a podcast from Figure 1 about how doctors think.
I’m Dr. Raj Bhardwaj.
This season, we’re doing something different. We’re taking you inside the minds of doctors who perform an essential – and often lifesaving – service in healthcare: abortion.
Throughout this series, you’ll hear from obstetricians inside Cleveland Clinic.
They’ll tell you about their patients.
For some, abortion saved their life. While for others, it safeguarded their emotional health, sparing them heartache and financial ruin.
We’ll talk about abortion as it affects physical and mental health.
Today, a case from Dr. Stacey Erhenberg, a maternal fetal medicine specialist at Cleveland Clinic in Cleveland, Ohio.
CHAPTER 1 — CASE STUDY
Dr. Stacey Ehrenberg: I first met this patient when she came to see us after an ultrasound. She was, average patient, middle class, working kind, sweet, lovely. Always with a smile on her face.
Dr. Bhardwaj: The concern with this patient was that her placenta did not look normal.
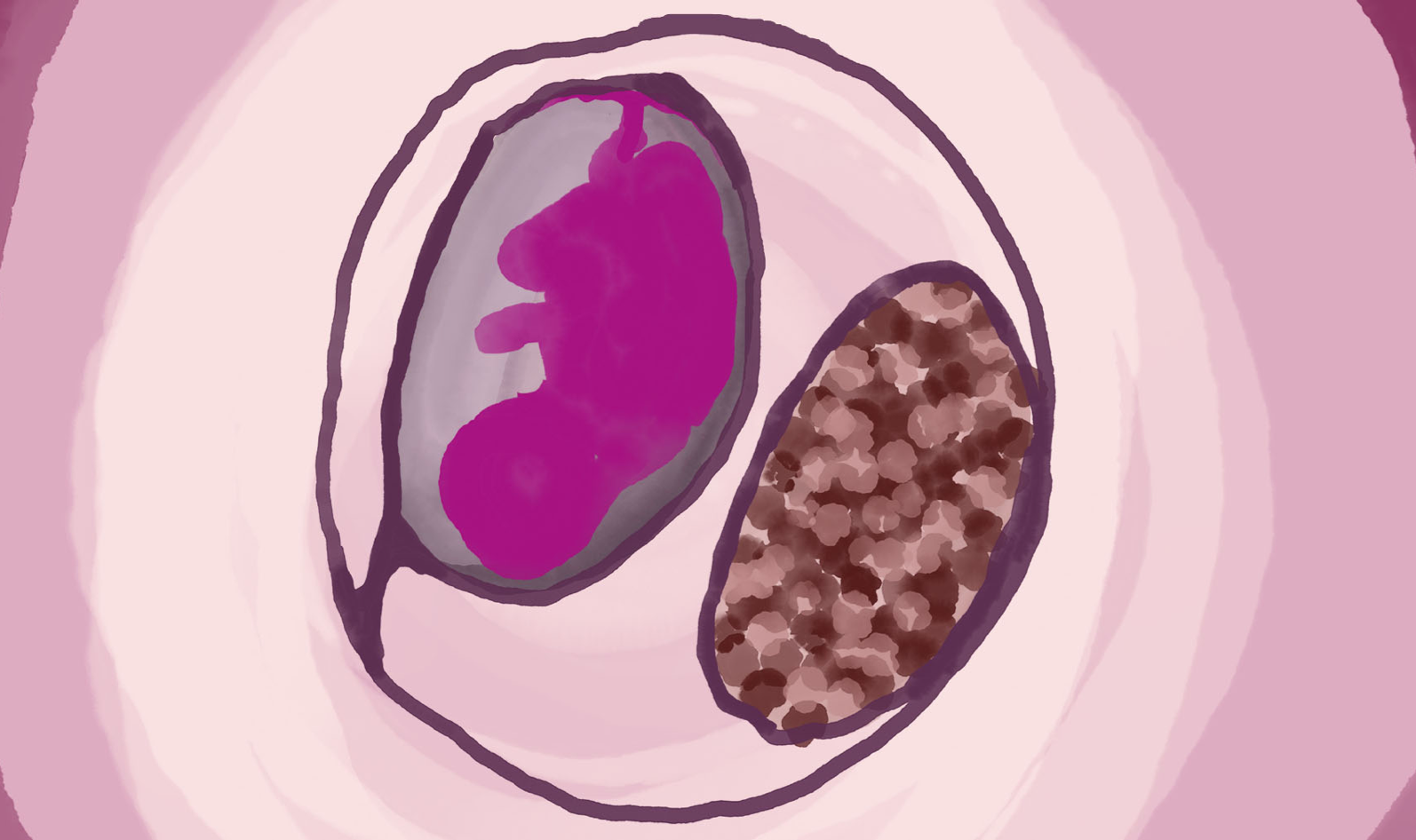
Dr. Ehrenberg: I noticed that not only was there an abnormally appearing placenta, but there was also a live pregnancy that looked completely normal and we diagnosed her with a twin pregnancy with a normal intrauterine pregnancy and something called a molar pregnancy.
Dr. Bhardwaj: A molar pregnancy is when the placenta doesn’t form properly. Instead of developing into a placenta, cells become a benign tumor, with the potential to become cancerous.
The twin with the abnormal placenta was not going to survive… but what about the other one…?
Dr. Ehrenberg: She also had a viable intrauterine pregnancy. We talked to her about the risk of continuation, which includes things like hypertension very early in the pregnancy, something called mirror syndrome, where you get hypertension and the patient starts swelling in different areas of the body and that can become life threatening.
We talked to her about bleeding. When the abnormal tissue is removed, there can be pretty significant bleeding involved. So those are the risks of continuing the pregnancy.
Dr. Bhardwaj: And Dr. Ehrenberg talked to her about the risks of abortion.
Dr. Ehrenberg: The risks of discontinuing the pregnancy are the risks of any procedure that we would do in the hospital, bleeding, infection, damage to the surrounding organs, the bowel and bladder are close by to where we operate. Damage to the uterus as possible. And all those things typically happen about less than 1% of the time. And so after giving her options, We said, okay, what would you like to do? Regardless of what you choose, we are here for you. We are gonna support you.
Dr. Bhardwaj: The patient chose to continue her pregnancy.
Dr. Ehrenberg: So we supported her through that and decided that we wanted to see her every week for an ultrasound and for blood pressure measurements. So we would check on her wellbeing and check on the wellbeing of the fetus and check on the molar pregnancy to see how much it’s grown.
Dr. Bhardwaj: Dr. Ehrenberg and her team continued to monitor the patient weekly, knowing that the odds of life-threatening complications were high.
Dr. Ehrenberg: I really watched her struggle throughout the pregnancy knowing that she knew that at some point the scale was gonna tip and that this would no longer be safe for her to continue. Her hope, as was ours, that she would be able to get far enough in pregnancy where the baby would be able to survive. She knew that this would probably be an extremely premature baby, but she was willing to take that risk to start her family.
Dr. Bhardwaj: When the patient was 19-weeks pregnant, she came to see Dr. Ehrenberg. It was an emergency.
Dr. Ehrenberg: She came in with mirror syndrome. I think this is one of the reasons I became a high risk obstetrician because I get to know my patients so well. I see them so often that I can look at them and tell something’s not right, and that was the feeling I got that day when she walked in. I took one look at her and she didn’t even have to say anything.
I didn’t need vital signs. I didn’t need to do a physical exam to know something wasn’t right. We got vital signs on her and I did a physical exam, and it was very clear to me that she had mirror syndrome and then we had to have the very difficult conversation that we knew that the baby was not yet viable, but it was no longer safe for her to remain pregnant.
She had severely elevated blood pressures. She was edematous all over, and we had to have the difficult conversation with her that the pregnancy was no longer safe to continue and is now life threatening to her. I can’t remember the exact dialogue. It’s more the feeling that I remember. We understood what this pregnancy meant to her. When we saw her blood pressures were elevated, and you could look at her from across the room and know that something wasn’t right
And you could see in her eyes that she knew that already. She knew that something was not right. She was devastated. We were devastated and of course worried for her health and wellbeing at this point. Our heart went out to her. Watching her so strongly desire to start her family knowing what she was risking. It really is an amazing thing that she was doing for this pregnancy and watching her struggle each week and all of us really hoping that we could get her to a point where the baby could survive was all of our goal. And I think we were all devastated when we weren’t able to do that for her and devastated for her and her family.
So the conversation was just heartbreaking. It is the hardest part of my job to have to tell a woman that we can’t continue a pregnancy, or that a pregnancy is not gonna end with a healthy mom and a healthy baby. we had to have the difficult conversation with her that the pregnancy was no longer safe to continue and is now life threatening to her.
Dr. Bhardwaj: In this situation, the risks of continuing the pregnancy were life-threatening.
Dr. Ehrenberg: She could have had a seizure at any moment. She could have pulmonary edema where fluid comes into her lungs. She could go into heart failure. She can have a stroke, she could die.
Dr. Bhardwaj: They reviewed the surgical options.
Dr. Ehrenberg: We opted for a dilation and evacuation where we went back to the operating room, made her comfortable with anesthesia, and then gently removed both the live, at that point, the intrauterine pregnancy and the molar pregnancy all at once.
Dr. Bhardwaj: But there were serious complications.
Because a molar pregnancy isn’t attached to the uterus, extensive bleeding is likely during this procedure.
Dr. Ehrenberg: When we started to remove the molar pregnancy, she had such severe hemorrhage and became hypotensive.
Dr. Bhardwaj: The patients hemorrhage was so severe it caused kidney failure.
Dr. Ehrenberg: When a patient loses a significant amount of blood once, their vital organs are not perfused in the way that they are. The normal amount of oxygen and nutrients that are going to the organs is not normal. So the body has to prioritize where they’re gonna send oxygen and nutrients when it has a limited supply. So it’s gonna prioritize the most important organs, the brain, the heart, and typically the adrenal glands, which is where a lot of our hormones are made. The blood flow is not gonna go to the kidneys as much as we would like because that’s not as much of a vital organ as the heart and the brain and the adrenal glands. So the kidneys, when they have a decrease in oxygen and nutrients, they stop working and it can be a complete shutdown, or it can be a partial shutdown, and the kidneys need time to recover.
Dr. Bhardwaj: Luckily this woman was otherwise healthy so she survived the extreme blood loss.
Dr. Ehrenberg: Fortunately she was able to make a full recovery.
CHAPTER 2 — LESSONS
Dr. Ehrenberg: As a high risk obstetrician, many patients’ faces flash through my mind. These women, they stick with me. They’re often my patients again and again through future pregnancies. It’s women and families who have had to deal with complications in pregnancy. A lot of this gets presented as black and white, that this issue is very black and white. It’s right, or it’s wrong, it’s black or it’s white and there’s a lot of gray.
And these pregnancy complications are so complex. The physical aspects of it, the emotional aspects of it, the financial aspects of it. They are complex and if you are not the one going through it, it’s so hard to understand what’s going on and what’s right in this specific situation. So I really just would love to see more kindness towards other people, more tolerance towards other people, more understanding that we don’t understand all the time where other people are coming from and what they’ve been through. In all situations, not just in healthcare.
Dr. Bhardwaj: Thanks to Dr. Ehrenberg for speaking with us.
This is DDx, a podcast by Figure 1.
Figure 1 is an app that lets doctors share clinical images and knowledge about difficult to diagnose cases.
I’m Dr. Raj Bhardwaj, host and story editor of DDx.
Head over to figure1.com/ddx, where you can find full show notes, photos and speaker bios.
This season of DDx is sponsored by Cleveland Clinic.
Cleveland Clinic is consistently ranked as one of the nation’s top hospitals for gynecologic care, by U.S. News & World Report. Learn more from Cleveland Clinic Women’s Health experts at consult qd dot cleveland clinic dot org.
Thanks for listening!